Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (27 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
11.32Mb size Format: txt, pdf, ePub
•
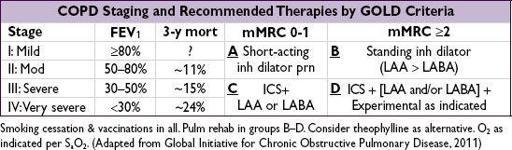
Bronchodilators
(
first-line therapy
):
anticholinergics
, β
2
-agonists (BA), theophylline
Long-acting (LA) anticholinergic (LAA, tiotropium): ↓ exac., ↓ admit, ↓ resp failure (
NEJM
2008;359:1543), better than ipratropium or LABA as mono Rx (
NEJM
2011;364:1093)
LABA: ~15% ↓ in exacerbations, ↓ FEV
1
decline, trend toward ↓ mort. (
NEJM
2007;356:775)
LABA + inh steroid: ? ↓ mort. (
NEJM
2007;356:775;
AJRCCM
2008;177:19)
LAA + LABA + inh steroid: ↑ FEV
1
, ↓ COPD admits (
Annals
2007;146:545)
•
Corticosteroids
(inhaled, ICS): ~20% ↓ in exacerb if FEV
1
<2.0 L (
Chest
2009;136:1029) may slow ↓ FEV
1
, but more so in combo with LABA (
NEJM
2007;356:775); ↑ in PNA (not seen w/ budesonide;
Lancet
2009;374:712); no Δ in mort. w/ ICS alone (
NEJM
2007;356:775)
• Antibiotics: daily azithro ↓ exacerb, but not yet routine (
NEJM
2011;365:689 & 2012;367:340)
• Mucolytics: no Δ FEV
1
, but ? ↓ exacerbation rate (
Lancet
2008;371:2013)
•
Oxygen
: if P
a
O
2
≤55 mmHg or S
a
O
2
≤89% (during rest, exercise or sleep) to prevent cor pulmonale; only Rx proven to ↓ mortality (
Annals
1980;93:391;
Lancet
1981;i:681)
•
Prevention
: Flu/Pneumovax; smoking cessation (eg, varenicline, bupropion) → 50% ↓ in lung function decline (
AJRCCM
2002;166:675) and ↓ long-term mortality (
Annals
2005;142:223)
• Rehabilitation: ↓ dyspnea and fatigue, ↑ exercise tolerance, ↓ QoL (
NEJM
2009;360:1329)
• Experimental
Lung volume reduction surgery: ↑ exer. capacity, ↓ mort.
if
FEV
1
>20%, upper-lobe, low exer. capacity (
NEJM
2003;348:2059); bronchoscopic w/ endobronchial valves w/ mixed benefits: ↑ lung fxn but ↑ PNA, exacerb, hemoptysis (
NEJM
2010;363:1233)
Roflumilast (PDE-4 inhibitor): ↑ FEV
1
when added to standard Rx (
Lancet
2009;374:685&695)
Nocturnal BiPAP: may improve survival, ? decrease QoL (
Thorax
2009;64:561)
• Lung transplant: ↑ QoL and ↓ sx (
Lancet
1998;351:24), ? survival benefit (
Am J Transplant
2009;9:1640)
Staging and prognosis
•
FEV
1
: 50–80% predicted → 3-y mort. ~11%; 30–50% → ~15%; <30% → ~24%
•
BODE
10-pt scale (
Lancet
2009;374:704); HR 1.62 for resp mort., 1.34 mort. for each 1-pt ↑
B
MI: ≤21 (+1)
O
bstruction (FEV
1
): 50–64% (+1), 36–49% (+2), ≤35% (+3)
D
yspnea (MMRC scale): walking level (+1), after 100 yd (+2), with ADL (+3)
E
xs capacity (6-min walk): 250–349 m (+1), 150–249 (+2), ≤149 (+3)
superior to FEV
1
(
NEJM
2004;350:1005); can predict survival from LVRS (
Chest
2006;129:873)
• mMRC score: ≥2 defined as walking slowly b/c breathlessness or having to stop to catch breath walking level
• Ratio of diam PA/aorta >1 associated with ~3× ↑ risk of exacerbations (
NEJM
2012;367:913)
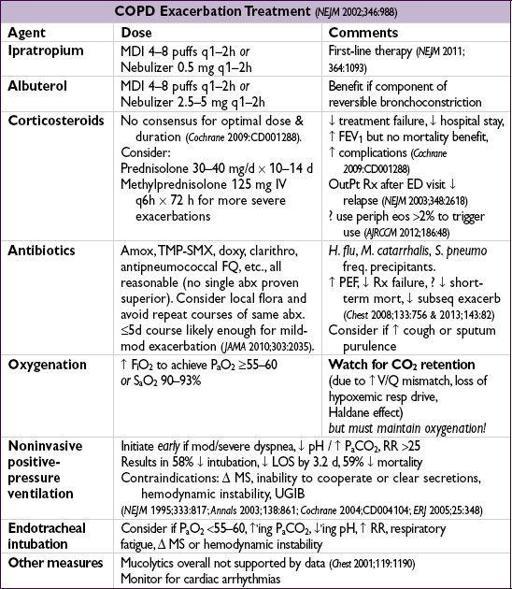
EXACERBATION
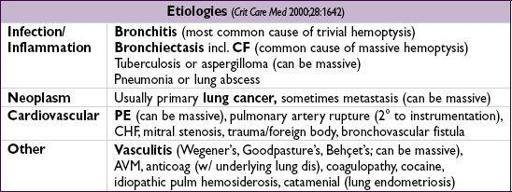
HEMOPTYSIS
Definition and pathophysiology
• Expectoration of blood or blood-streaked sputum •
Massive hemoptysis
: ~>600 mL/24–48 h; gas exchange more important than blood loss • Massive hemoptysis usually from tortuous or invaded
bronchial arteries
Diagnostic workup
• Localize bleeding site
Rule out GI or ENT source
by exam, history; may require endoscopy
Pulmonary source: determine whether
unilateral or bilateral, localized or diffuse, parenchymal or airway
by CXR or chest CT, bronchoscopy if necessary
• PT, PTT, CBC to rule out
coagulopathy
• Sputum culture/stain for bacteria, fungi and AFB; cytology to
r/o malignancy
• ANCA, anti-GBM, urinalysis to ✓ for
vasculitis
or
pulmonary-renal syndrome
Treatment
• Mechanism of death is asphyxiation not exsanguination; maintain gas exchange, reverse coagulation and treat underlying condition; cough supp. may ↑ risk of asphyxiation • Massive hemoptysis: put bleeding side dependent; selectively intubate nl lung if needed
Angiography:
Dx & Rx (vascular occlusion balloons or
selective embol of bronchial art
)
Rigid bronchoscopy:
allows more interventional options (electrocautery, laser) than flex. Surgical resection
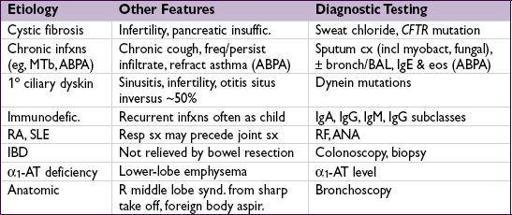
BRONCHIECTASIS
Definition and epidemiology
(
NEJM
2002;346:1383)
• Obstructive airways disease of bronchi and bronchioles, chronic transmural inflamm w/ airway dilatation and thickening, collapsibility, mucus plugging w/ impaired clearance • Frequency:>
; in the U.S. more frequent in Asian Americans (
Chest
2012;142:432)
Initial workup
• H&P: cough, dyspnea, copious sputum production, ± hemoptysis, inspiratory “squeaks”
• CXR: scattered or focal; rings of bronchial cuffing; “tram track” of dilated, thick airways • PFTs: obstructive pattern • Chest CT: dilation and thickening of airways; ± cystic changes, infiltrates, adenopathy
Treatment
• Treat underlying condition; mucolytics & bronchodilators • Antibiotics: CF Pts often have multiple drug-resistant organisms (
Pseudomonas
,
Burkholderia cepacia
,
S. aureus
) and require IV antibiotics during exacerbations. Azithro shown to ↓ exacerb. in non-CF bronchiectasis (
Lancet
2012;380:660;
JAMA
2013;309:1251).
• Emerging data on gene-based targeted therapies in CF (
NEJM
2011;365:1663)
SOLITARY PULMONARY NODULE
Principles
• Definition: single, <3 cm, surrounded by normal lung, no LAN or pleural effusion • Often “incidentalomas,” esp with ↑ CT use, but may still be early, curable malignancy
Other books
Her Wounded Warrior by Kristi Rose
Witness the Dead by Craig Robertson
Rival Love by Natalie Decker
Lo! by Charles Fort
Parasite Soul by Jags, Chris
A Fairy Tale by Jonas Bengtsson
Unearthly Power by R. K.
Lo Michael! by Grace Livingston Hill
Un manual de vida by Epicteto
Poison Ink by Christopher Golden