Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (23 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
6.02Mb size Format: txt, pdf, ePub
cardiac: HF (↑ JVP, displ. PMI, S
3
), murmurs, LVH (S
4
, LV heave), PHT (RV heave, ↑ P
2
)
vascular: ✓ for asymmetric pulses, carotid/vertebral/subclavian bruits; carotid sinus massage to assess for carotid hypersensitivity (if no bruits)
neurologic exam: focal findings, evidence of tongue biting; FOBT
•
ECG
(abnormal in
50%, but only definitively identifies cause of syncope in
10%)
Conduction: SB, sinus pauses/sinus arrhythmia, AVB, BBB/IVCD
Arrhythmia: ectopy, ↓ QT, preexcitation (WPW), Brugada, e wave (ARVC), SVT/VT
Ischemic changes (new or old): atrial or ventricular hypertrophy
Other diagnostic studies (consider based on results of H&P and ECG)
• Ambulatory ECG monitoring: if suspect arrhythmogenic syncope
Holter monitoring (continuous ECG 24–48 h): useful if
frequent
events arrhythmia + sx (4%); asx but signif. arrhythmia (13%); sx but no arrhythmia (17%)
Event recorder (activated by Pt to record rhythm strip): limited role as only useful if established prodrome (because must be Pt activated)
Loop recorders (continuously saves rhythm, ∴ can be activated
after
an event): useful for episodes (including w/o prodrome) likely to occur w/in month.
Implantable
loop recorders (inserted SC; can record up to 3 y): useful for infrequent episodes (<1/mo); recommended for recurrent syncope w/o prodrome
• Echo: consider to r/o structural heart disease (eg, CMP [incl HCMP & ARVC], valvular disease [incl AS, MS, MVP], myxoma, amyloid, PHT, ± anomalous coronaries) • ETT: esp. w/ exertional syncope; r/o ischemia-or catecholamine-induced arrhythmias • Cardiac catheterization: consider if noninvasive tests suggest ischemia • Electrophysiologic studies (EPS): consider in high-risk Pts in whom tachy or brady etiology is strongly suspected, but cannot be confirmed;
50% abnl (inducible VT, conduction abnormalities) if heart disease, but ? significance
3–20% abnl if abnl ECG; <1% abnl if normal heart and normal ECG (
Annals
1997;127:76)
• ? Tilt table testing: utility is debated due to poor Se/Sp/reproducibility; consider only if vasovagal dx suspected but can’t be confirmed by hx • Cardiac MRI: helpful to dx ARVC if suggestive ECG, echo (RV dysfxn) orFHx of SCD
• Neurologic studies (cerebrovascular studies, CT, MRI, EEG): if H&P suggestive; low yield
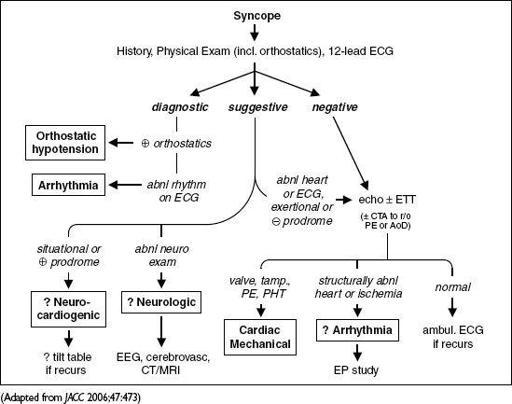
Figure 1-6
Approach to syncope
High-risk features (usually admit w/ telemetry & testing;
J Emerg Med
2012;42:345)
• Age >60 y, h/o CAD, HF/CMP, valvular or congenital heart dis., arrhythmias, FHx SCD
• Syncope c/w cardiac cause (lack of prodrome, exertional, resultant trauma) or recurrent • Complaint of chest pain or dyspnea; abnl VS or cardiac exam • ECG suggesting tachy or brady-induced syncope; Pt w/ PPM/ICD
Treatment
• Arrhythmia, cardiac mechanical or neurologic syncope: treat underlying disorder • Vasovagal syncope: no proven benefit for midodrine, fludrocortisone, disopyramide, SSRI ? 16 oz of H
2
O before at-risk situations (
Circ
2003;108:2660)
no proven benefit w/ bB (
Circ
2006;113:1164)
? benefit w/ PPM if ≥3 episodes/2y & loop recorder w/ asystole >3 sec (
Circ
2012;125:2566)
• Orthostatic syncope: volume replete (eg, 500 mL PO q a.m.); if chronic → rise from supine to standing
slowly
, compressive stockings, midodrine, fludrocortisone, high Na diet
Prognosis (
Ann Emerg Med
1997;29:459;
NEJM
2002;347:878)
• 22% overall recurrence rate if idiopathic, else 3% recurrence • Cardiac syncope: 2-fold ↑ in mort., 20–40% 1-y SCD rate, median survival ~6 y • Unexplained syncope w/ 1.3-fold ↑ in mort., but noncardiac or unexplained syncope w/ nl
ECG, no h/o VT, no HF, age <45 → low recurrence rate and <5% 1-y SCD rate
• Vasovagal syncope: Pts not at increased risk for death, MI or stroke • ✓ state driving laws and MD reporting requirements. Consider appropriateness of Pt involvement in exercise/sport, operating machinery, high-risk occupation (eg, pilot).
INTRACARDIAC DEVICES
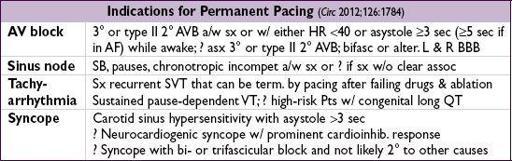
Cardiac resynch therapy (CRT)/Biventricular (BiV) pacing (Circ 2012;126:1784)
• 3-lead pacemaker (RA, RV, coronary sinus to LV); R>S in V
1
suggests approp LV capture
• Synchronize & enhance LV fxn (↑ CO, ↓ adverse remodeling)
•
Indic
: LVEF ≤35% + NYHA II–IV despite med Rx + SR + LBBB ≥150 ms (also reasonable if
either
LBBB ≥120 ms
or
no LBBB but QRS ≥150 ms + NYHA III–IV); consider in AF, but rate cntl → ~100% vent capture; ? NYHA I w/ LVEF ≤30% + LBBB ≥150 ms; ? EF ≤50% w/ AVB + indic for PPM (
NEJM
2013;368:1585)
•
Benefits
: ↓ HF sx, ↓ HF hosp., ↑ survival (NEJM 2005;352:1539; 2010;363:2385)
Implantable cardiac defibrillator (ICD) (NEJM 2003;349:1836; JACC 2009;54:747)
• RV lead: defib & pacing (± antitachycardia pacing [ATP] = burst pacing > VT rate to stop VT); ± RA lead for dual chamber PPM. Wearable vest & SC ICD exist (Circ 2013;127:854).
•
Pt selection
(NEJM 2004;350:2151 & 351:2481; 2005;352:225; 2009;361:1427; Circ 2012;126:1784)
2° prevention: survivors of VF arrest, unstable VT w/o reversible cause (NEJM 1997;337:1576); structural heart disease & spontaneous sustained VT (even if asx)
1° prevention: LVEF ≤30% & post-MI
or
LVEF ≤35% & NYHA II-III (wait: ≥40 d if post-MI, ? until stabilized on meds for NICMP, or if presumed reversible)
or
LVEF ≤40% & inducible VT/VF;
life expectancy must be
>
1
y
; consider for HCM, ARVC, Brugada, sarcoid, LQTS, Chagas or congenital heart disease if risk factors for SCD
•
Benefits
: ↓ mortality from SCD c/w antiarrhythmics or placebo
•
Risks:
inapprop shock in ~15–20% at 3 y (most commonly d/t misclassified SVT); infxn
• ICD discharge: ✓ device to see if approp; r/o ischemia; 6-mo driving ban (✓ state law); if recurrent VT, ? drug Rx (eg, amio + bB, JAMA 2006;295:165) or VT ablation (NEJM 2007;357:2657); ablation at time of ICD ↓ risk of VT by 40% (Lancet 2010;375:31)
Device infection (Circ 2010;121:458; JAMA 2012;307:1727; NEJM 2012;367:842)
• Presents as
pocket infection
(warmth, erythema, tenderness) and/or
sepsis w
/
bacteremia
Other books
Wicked Thing (C.O.A Series Book 2) by Kim Cormack
Dread on Arrival by Claudia Bishop
Fire and Sword by Scarrow, Simon
Hunt for the Panther 3 (9781101610923) by Delaney, Rachelle; Guerlais, Gerald (ILT)
Losing You (Stars On Fire Book 4) by Ryleigh Andrews
In Her Way by Eryn Scott
Mountain Homecoming by Sandra Robbins
Just For Now (A Flirting With Trouble Novel) by Annie Kelly
Cinderella: Ninja Warrior by Maureen McGowan
Lone Rider (Motorcycle Club Romance) by Lawson, Kelly