Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (29 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.4Mb size Format: txt, pdf, ePub
•
Amiodarone
(~10%; dose & duration depend.): chronic interstitial pneumonia ↔ ARDS; bx → vacuolized Mf w/ lamellar inclusions on EM; Rx: d/c amio, give steroids • Other drugs: nitrofurantoin, sulfonamides, thiazides, INH, hydralazine, gold • Chemo: bleomycin (triggered by hyperoxia), busulfan, cyclophosphamide, MTX,
etc.
• XRT: COP/BOOP w/ sharply linear, nonanatomic boundaries; DAH
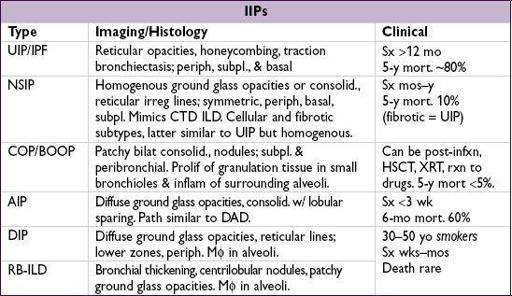
Idiopathic interstitial pneumonias (IIPs)
(
AJRCCM
2005;172:268)
• Definition:
ILD of unknown cause
; dx by radiographic, histologic and clinical features
UIP, usual interstitial PNA (IP); IPF, idiopathic pulm fibrosis (
Lancet
2011;378:1949); NSIP, nonspecific IP; COP, cryptogenic organizing PNA; BOOP, bronchiolitis obliterans w/ organizing PNA; AIP, acute IP (Hamman-Rich syndrome); DIP, desquamative IP; RB-ILD, resp bronchiolitis-assoc ILD.
• Rx for UIP/IPF: ?? NAC (
NEJM
2005;353:2229); pred + AZA harmful (
NEJM
2012;366:1968)
Experimental: tyrosine kinase inhib (
NEJM
2011;365:1079); pirfenidone (
Lancet
2011;377:1760; not avail in U.S.); ? sildenafil (
NEJM
2010;363:621); thalidomide for cough (
Annals
2012;157:398)
• Steroids for other IIPs: NSIP (esp. cellular type) and COP (
AJRCCM
2000;162:571); ? benefit for AIP and DIP/RB-ILD (for which Pts should stop smoking)
Environmental & occupational exposures
(
NEJM
2000;342:406;
Lancet
2012;379:2008)
•
Pneumoconioses
(inorganic dusts)
Coal worker’s: upper lobe coal macules; may progress to massive fibrosis
Silicosis: upper lobe opacities ± eggshell calcification of lymph nodes; ↑ risk of TB
Asbestosis: lower lobe fibrosis, calcified pleural plaques, DOE, dry cough, rales on exam. Asbestos exposure also → pleural plaques, benign pleural effusion, diffuse pleural thickening, rounded atelectasis, mesothelioma, lung Ca (esp. in smokers).
Berylliosis: multisystemic granulomatous disease that mimics sarcoidosis
•
Hypersensitivity pneumonitides
(organic dusts): loose, noncaseating
granulomas
Antigens: farmer’s lung (spores of thermophilic actinomyces); pigeon fancier’s lung (proteins from feathers and excreta of birds); humidifier lung (thermophilic bacteria)
Collagen vascular diseases
(
NEJM
2006;355:2655)
•
Rheumatologic disease
Scleroderma: fibrosis in
67%; PHT seen in
10% of CREST Pts
PM-DM: ILD & weakness of respiratory muscles; MCTD: PHT & fibrosis
SLE & RA: pleuritis and pleural effusions more often than ILD; SLE can cause DAH
•
Vasculitis
(can p/w
DAH
)
Wegener’s granulomatosis (c-ANCA) w/ necrotizing granulomas
Churg-Strauss syndrome (c-or p-ANCA) w/ eosinophilia & necrotizing granulomas
Microscopic polyangiitis (p-ANCA) w/o granulomas
•
Goodpasture’s syndrome
= DAH + RPGN; typically in smokers;anti-GBM in 90%
•
Lymphangioleiomyomatosis
(LAM): cystic, ↑ in, Rx w/ sirolimus (
NEJM
2011;364:1595)
Pulmonary infiltrates w/ eosinophilia (PIE)
=
eos on BAL ± periph. blood
•
Allergic bronchopulmonary aspergillosis
(
ABPA
): allergic reaction to
Aspergillus
Criteria: asthma, pulm infiltrates (transient or fixed), skin rxn & serum precipitins to
Aspergillus
, ↑ IgE to
Aspergillus
& total (>1000), ↑ eos, central bronchiectasis
Rx: steroids ± itraconazole for refractory cases (
NEJM
2000;342:756)
• Löffler’s syndrome: parasites/drugs → transient pulm infilt + cough, fever, dyspnea, eos • Acute eosinophilic PNA (AEP): acute hypox febrile illness; Rx: steroids, tobacco cessation • Chronic eosinophilic pneumonia (CEP): “photonegative” of CHF, typically in women • Other: Churg-Strauss syndrome; hypereosinophilic syndrome
Miscellaneous
• Pulm alveolar proteinosis (PAP): accum of surfactant-like phospholipids;smokers; white & gummy sputum; BAL milky fluid (
NEJM
2003;349:2527); Rx w/ lung lavage & GMCSF
• Langerhans cell granulomatosis (LCG): youngsmokers; apical cysts; PTX (25%) • Lymphocytic interstitial PNA: polyclonal B-cell infiltration (? lymphoma); Rx: steroids
PLEURAL EFFUSION
Pathophysiology
•
Systemic factors
(eg, ↑ PCWP, ↓ oncotic pressure) →
transudative
effusion •
Local factors
(ie, Δ pleural surface permeability) →
exudative
effusion
Transudates
•
Congestive heart failure
(
40%
): 80% bilateral, ± cardiomegaly on CXR occasionally exudative (esp. after aggressive diuresis or if chronic), but ~75% of exudative effusions in CHF Pts found to have non-CHF cause (
Chest
2002;122:1518) •
Constrictive pericarditis
(knock on exam, calcification or thickening on imaging) •
Cirrhosis
(“hepatic hydrothorax”): diaphragmatic defect w/ passage of ascitic fluid often right-sided (
2
/
3
) & massive (even w/o marked ascites) • Nephrotic syndrome: usually small, bilateral, asymptomatic (r/o PE b/c hypercoag) • Other: PE (usually exudate), malignancy (lymphatic obstruction), myxedema, CAPD
Other books
Storm Maiden by Mary Gillgannon
Enchanting Wilder by Cassie Graham
Gates to Tangier by Mois Benarroch
Wherever Grace Is Needed by Elizabeth Bass
With This Fling... by Kelly Hunter
ISS by Mains, L Valder, Mains, Laurie
The Royal Pursuit by Ruth Ann Nordin
Dragon Flight by Jessica Day George
Your Bed or Mine? by Candy Halliday