Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (24 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
6.93Mb size Format: txt, pdf, ePub
• Incidence ~2% over 5 y; if
S. aureus
bacteremia, infxn in ≥35%
• TTE/TEE used to help visualize complic. (eg, vegetation), but evenTEE does not r/o
• Treatment: abx and removal of system; Ppx: no rec for routine abx prior to invasive proc.
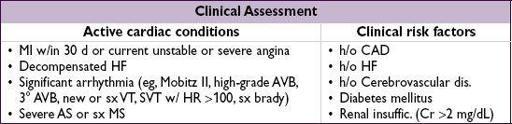
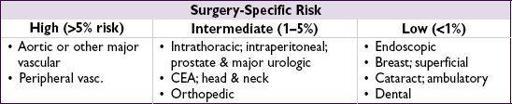
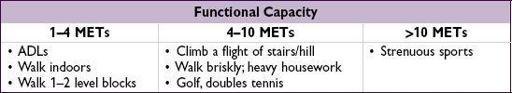
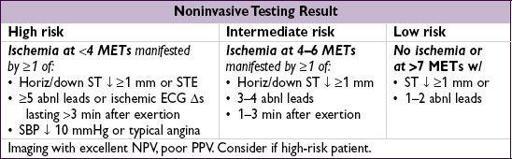
CARDIAC RISK ASSESSMENT FOR NONCARDIAC SURGERY
Preoperative evaluation
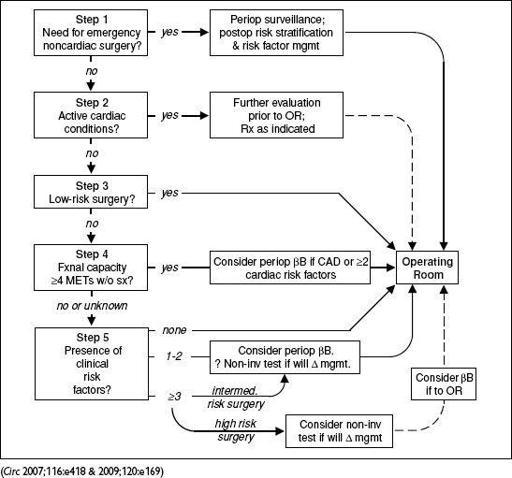
Figure 1-7
ACC/AHA approach to preoperative cardiovascular evaluation for noncardiac surgery
Preoperative testing and assessment
• ECG if ≥1 risk factor and planned vascular surgery or if known vascular disease and intermediate risk surgery. ? prior to any vascular surgery.
• TTE if dyspnea of unknown origin or if HF w/ ↑ dyspnea and no TTE in past 12 mo
• Stress test if active cardiac issues (see above) or vascular surgery w/ ≥3 risk factors & it will Δ mgmt. Overall low PPV to predict periop CV events.
• ? consider CXR and ECG in preop evaluation of severely obese Pts (Circ 2009;120:86)
• Comorbidity indices (eg, Charlson index) may predict mortality (Am J Med Qual 2011;26:461)
Pre- & perioperative management
•
Coronary revascularization
should be based on
standard indications
(eg, ACS, refractory sx, lg territory at risk). Has not been shown to Δ risk of death or postop MI when done prior to elective vasc. surgery based on perceived cardiac risk (NEJM 2004;351:2795) or documented extensive ischemia (AJC 2009;103:897), but systematic angio ↓ 2–5 y mortality in a vascular surgery trial ( JACC 2009;54:989).
• Continue ASA: ↓ MACE in Pts w/ cardiac risk factors (Br J Anaesth 2010;104:305)
• Given need for dual antiplatelet Rx after stenting, wait 4–6 wk after BMS and ideally >12 mo after DES before discontinuing ADP receptor blockade • If possible, wait >4–6 wk after MI (even ifETT or
ETT & revascularized). If no
revasc, wait 6 mo before elective surgery.
• Preop statins: ↓ ischemia & CV events in Pts undergoing vascular surg (NEJM 2009;361:980); may reduce AF, MI, LOS in statin-naïve Pts (Arch Surg 2012;147:181)
Perioperative
β
-blocker (Circ 2009;120:2123; JAMA 2010;303:551; Am J Med 2012;125:953)
• Conflicting evidence: some studies show ↓ death & MI (NEJM 1996;335:1713 & 1999;341:1789), another showed ↓ MI, but ↑ death & stroke and ↑ bradycardia/HoTN (Lancet 2008;371;1839) • ? consider if CAD,stress test, or ≥2 cardiac risk factor, esp. if vascular surgery • Ideally initiate
weeks
prior to surgery and titrate slowly and carefully to achieve desired individual HR and BP goal (? HR ~55–65). Avoid bradycardia and hypotension. Do not discontinue bB abruptly postop, as may cause sympathetic activation from withdrawal.
Postoperative monitoring
• ✓ Postop ECG if known CAD or high-risk surgery. Consider if >1 risk factor for CAD.
• ✓ Postop troponin only if new ECG Δs or chest pain suggestive of ACS
PERIPHERAL ARTERY DISEASE (PAD)
Clinical features
• Prev. ↑ w/ age: <1% if <40 y, ~15% if ≥70 y; risk factors incl.
smoking
,
DM
, HTN, chol
•
Claudication
(dull ache, often in calves) precip by walking and relieved by stopping (vs. spinal stenosis, qv); Leriche synd = claudication, ↓ or femoral pulses, & erectile dysfxn
•
Critical limb ischemia (CLI)
:
rest pain
(↑ w/ elevation b/c ↓ perfusion),
ulcer
(typically at pressure foci, often dry; in contrast, venous ulcers are more often at medial malleolus, wet, and with hemosiderin deposition) or
gangrene
, due to PAD, and >2-wk duration (implies chronicity vs. acute limb ischemia, see below)
Diagnosis
• ↓ peripheral pulses; other signs of chronic PAD: hair loss, skin atrophy, nail hypertrophy
• Ankle:brachial index (ABI): nl 1–1.4; borderline 0.91–0.99; abnl ≤0.90; if >1.4, non-dx possibly due to calcified noncompressible vessel → ✓ PVR. If ABI abnl → segmental ABI w/ PVR to localize disease. Ifsx but nl ABI, ✓ for ↓ lower extrem BP after exercise.
Other books
Taking You by Jessie Evans
Wild Child by Boyle, T. C.
Louise Rennison_Georgia Nicolson 04 by Dancing in My Nuddy Pants
Forbidden Love by Maura Seger
Casca 13: The Assassin by Barry Sadler
Bloodraven by Nunn, P. L.
Apathy and Other Small Victories by Neilan, Paul
The Dragon Wicked by B. V. Larson
The Mysterious Howling by Maryrose Wood
Caine's Reckoning by Sarah McCarty