Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (25 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
5.73Mb size Format: txt, pdf, ePub
• Duplex arterial U/S; CTA w/ distal run-off; MRA or angio
Treatment (
JACC
2013;61:1555; JAMA 2013;309:453)
• Risk factor modification. Supervised exercise Rx. Screen for CAD.
• Cilostazol (if no HF) & ? ACEI to ↓ sx. ASA or clopi to ↓ D/MI/stroke if claud. or ABI <0.9.
• Revasc if CLI or limiting/refractory claudication
Acute limb ischemia (ALI)
• Sudden decrement in limb perfusion that threatens viability;
viable
(no immed threat of tissue loss): audible art. Doppler signals, sensory & motor OK
threatened
(salvage requires prompt Rx): loss of arterial Doppler signal, sensory or motor
• Etiologies: embolism > acute thrombosis (eg, athero, APLA, HITT), trauma to artery
• Clinical manifestations (
6 Ps
): pain (distal to proximal, ↑ in severity), poikilothermia, pallor, pulselessness, paresthesias, paralysis
• Testing: thorough pulse & neuro exam; arterial Doppler; angiography, either CT w/ bilateral run-off through feet or arteriography
• Urgent consultation w/ vascular medicine and/or vascular surgery
• Treatment: immediate anticoagulation ± intraarterial lytic; angioplasty or surgery
NOTES
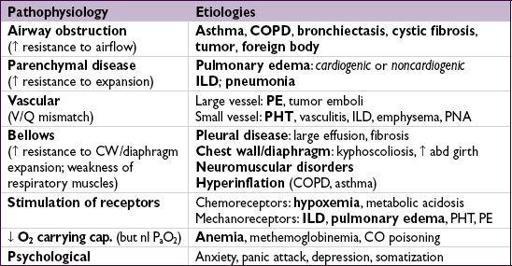
DYSPNEA
Evaluation
• History: quality of sensation, tempo, positional dependence, exac./allev. factors, exertion
• Cardiopulmonary exam, S
a
O
2
, CXR (see Appendix & Radiology inserts), ECG predictors of CHF: h/o CHF, PND, S
3
, CXR w/ venous congestion, AF (
JAMA
2005;294:1944) dyspnea w/ nl CXR → CAD, asthma, PE, PHT, early ILD, anemia, acidosis, NM disease
• Based on results of initial evaluation: PFT, chest CT, TTE, cardiopulmonary testing
•
BNP & NT-proBNP
↑ in CHF (also ↑ in AF, RV strain from PE, COPD flare, PHT, ARDS) BNP <100 pg/mL to r/o CHF (90% Se), >400 to r/i (
NEJM
2002;347:161)
NT-proBNP <300 pg/mL to r/o CHF (99% Se); age-related cut points to r/i: >450 pg/mL (<50 y), >900 (50–75 y), >1800 (>75 y) (
EHJ
2006;27:330)
↑ in chronic heart failure, ∴ need to compare to known “dry BNP”
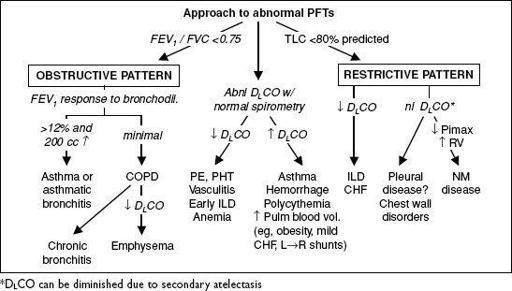
PULMONARY FUNCTION TESTS (PFTs)
•
Spirometry
: evaluate for obstructive disease
Flow-volume loops: diagnose and/or localize obstruction
Bronchodilator: indicated if obstruction at baseline or asthma clinically suspected
Methacholine challenge: helps dx asthma if spirometry nl, >20% ↓ FEV
1
→ asthma
•
Lung volumes
: evaluate for hyperinflation or restrictive disease including NM causes •
D
L
CO
: evaluates functional surface area for gas exchange; helps differentiate causes of obstructive and restrictive diseases and screens for vascular disease & early ILD
Figure 2-1 Approach to abnormal PFTs
ASTHMA
Definition and epidemiology
• Chronic inflam. disorder w/
airway hyperresponsiveness
+
variable airflow obstruction
• Affects
5% population;
85% of cases by age 40 y
Clinical manifestations
(
NEJM
2001;344:350)
• Classic triad =
wheezing
,
cough and dyspnea
; others include chest tightness, sputum; symptoms typically
chronic
with
episodic exacerbation
• Precipitants (
triggers
)
respiratory irritants
(smoke, perfume, etc.) &
allergens
(pets, dust mites, pollen, etc.)
infections
(URI, bronchitis, sinusitis)
drugs
(eg, ASA & NSAIDs via leukotrienes, bB via bronchospasm, MSO
4
via histamine) emotional stress, cold air, exercise (increase in ventilation dries out airways)
Physical examination
• Wheezing and prolonged expiratory phase • Presence of nasal polyps, rhinitis, rash →
allergic component
• Exacerbation → ↑ RR, ↑ HR, accessory muscle use, diaphoresis, pulsus paradoxus
Diagnostic studies
•
Peak exp flow
(
PEF
): ≥60 L/min ↑ after bronchodil or ≥20% diurnal variation c/w asthma. <80% personal best c/w poor control, <50% c/w severe exacerbation.
•
Spirometry
: ↓ FEV
1
, ↓ FEV
1
/FVC, coved flow-volume loop; lung volumes: ± ↑ RV & TLC
bronchodilator response (↑ FEV
1
≥12% & ≥200 mL) strongly suggestive of asthma methacholine challenge (↓ FEV
1
≥20%) if PFTs nl: Se >90% (
AJRCCM
2000;161:309)
• Sputum: eos >3% has 86% Se, 88% Sp; can also see
Curschmann’s spirals
(mucus casts of distal airways) and
Charcot-Leyden
crystals (eosinophil lysophospholipase) • Allergy suspected → consider ✓ serum IgE, eos, skin testing/RAST
Ddx
(“all that wheezes is not asthma … ”)
• Hyperventilation & panic attacks • Upper airway obstruction or inh foreign body; laryngeal/vocal cord dysfxn (eg, 2° to GERD) • CHF (“cardiac asthma”); COPD, bronchiectasis; ILD (including sarcoidosis); vasculitis; PE
“Asthma plus” syndromes
(
Lancet
2002;360:1313)
• Atopy = asthma + allergic rhinitis + atopic dermatitis • ASA-sensitive asthma (Samter’s syndrome) = asthma + ASA sensitivity + nasal polyps • ABPA = asthma + pulmonary infiltrates + allergic rxn to
Aspergillus
• Churg-Strauss = asthma + eosinophilia + granulomatous vasculitis
“Reliever” medications
(used prn to quickly relieve sx)
•
Short-acting
inh β
2
-agonists
(SABA): albuterol Rx of choice •
Short-acting
inh
anticholinergics
(ipratropium) ↑ β
2
-agonist delivery → ↑ bronchodilation
“Controller” meds
(taken daily to keep control)
(
NEJM
2009;360:1002)
• Inh
corticosteroids
(ICS): Rx of choice (
JAMA
2001;285:2583). PRN ? as good as daily for mild asthma (
NEJM
2005;352:1519 & 2007;356:2040). PO steroids may be needed for severely uncontrolled asthma, but avoid if possible b/c systemic side effects.
•
Long-acting
inh β
2
-
agonists
(LABA; eg, salmeterol): ↑ PEF when added to ICS (
Lancet
2009;374:1754). Except for exercise-induced asthma, should
not
be used w/o ICS (may ↑ mortality, esp. in African Americans) (
Chest
2006;129:15;
Annals
2006;144:904). Clinical relevance of β
2
-receptor pharmacogenetic interaction not validated (
Lancet
2009;374:1754).
•
Long-act
inh
anticholinergics
(LAA; eg, tiotropium): add-on if sx despite ICS (superior to ↑ ICS,to adding LABA;
NEJM
2010;363:1715) or if sx despite ICS+LABA (
NEJM
2012;367:1198) •
Nedocromil/cromolyn
: limited use in adults. Useful in young Pts, exercise-induced bronchospasm; ineffective unless used before trigger or exercise exposure.
•
Theophylline
: useful if hard to control sx; PO convenient, but high side-effect profile •
Leukotriene antagonists
(LTA): some Pts very responsive, esp. ASA-sens (
AJRCCM
2002;165:9) and exercise-induced (
Annals
2000;132:97). May be noninf to ICS initial Rx and LABA add-on Rx (
NEJM
2011;364:1695).
•
Anti-IgE
: for uncontrolled mod-to-severe allergic asthma (↑ IgE) on ICS ± LABA (
NEJM
2006;354:2689;
Annals
2011;154:573); not cost-effective for most Pts (
JACI
2007;120:1146)
Other
• Behavior modification: identify and avoid triggers; PPI w/o benefit (
NEJM
2009;360:1487) • Immunotherapy (eg, desensitization): may be useful if significant allergic component • TNF antagonists may be helpful in Pts w/ refractory asthma (
NEJM
2006;354:697) • Anti-IL5 (mepolizumab) ↓ exac. w/ sev asthma (
Lancet
2012;380:651), not yet FDA approved • Anti-IL13 (lebrikizumab) ↑ FEV
1
(
NEJM
2011;365:1088), not yet FDA approved • Bronchial thermoplasty (exp’tal): radiofrequency destruction of airway smooth muscle no Δ in FEV
1
, but ↓ in sx and # of exacerbations (
NEJM
2007;356:1327)
Principles of treatment
Other books
In Too Deep by Michelle Kemper Brownlow
Tales of Terror from the Black Ship by Chris Priestley
Son of Eden, a Paranormal Romance by Brianna Merrill
When He Dares by Emma Gold
The Dawn of Christmas by Cindy Woodsmall
At His Mercy by Masten, Erika
From the Mouth of the Whale by Sjon
When Hope Blossoms by Kim Vogel Sawyer
Lawnboy by Paul Lisicky
vN by Madeline Ashby