Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (30 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
7.83Mb size Format: txt, pdf, ePub
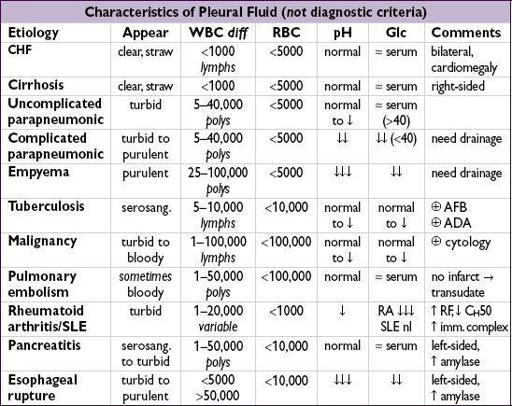
Exudates
•
Lung parenchymal infection
(
25%
)
bacterial (parapneumonic): can evolve along spectrum of
exudative
(but sterile) →
fibropurulent
(infected fluid) →
organization
(fibrosis & formation of rigid pleural peel). Common causes:
Strep pneumo, Staph aureus, Strep milleri, Klebsiella, Pseudomonas, Haemophilus, Bacteroides, Peptostreptococcus
, mixed flora in aspiration pneumonia.
mycobacterial: >50% lymphs 80% of the time, ADA >40, pleural bx ~70% Se
fungal, viral (usually small), parasitic (eg, amebiasis, echinococcosis, paragonimiasis)
•
Malignancy
(
15%
): primary lung cancer most common, metastases (esp. breast, lymphoma, etc.), mesothelioma (✓ serum osteopontin levels;
NEJM
2005;353:15) •
Pulmonary embolism
(
10%
): effusions in ~40% of PEs; exudate (75%) > transudate (25%); hemorrhagic—
must have high suspicion b/c presentation highly variable
•
Collagen vascular disease
: RA (large), SLE (small), Wegener’s, Churg-Strauss •
Gastrointestinal diseases
: pancreatitis, esophageal rupture, abdominal abscess • Hemothorax (Hct
eff
/Hct
blood
>50%): trauma, PE, malignancy, coagulopathy, leaking aortic aneurysm, aortic dissection, pulmonary vascular malformation • Chylothorax (triglycerides >110): thoracic duct damage due to trauma, malignancy, LAM
• Other:
post-CABG: left-sided; initially bloody, clears after several wks
Dressler’s syndrome (pericarditis & pleuritis post-MI), uremia, postradiation therapy
Asbestos exposure: benign;eosinophils
Drug-induced (eg, nitrofurantoin, methysergide, bromocriptine, amiodarone):eos
Uremia; post-XRT; sarcoidosis
Meigs’ syndrome = benign ovarian tumor → ascites & pleural effusion
Yellow-nail syndrome: yellow nails, lymphedema, pleural effusion, bronchiectasis
Diagnostic studies
•
Thoracentesis
(
NEJM
2006;355:e16)
Indications:
all effusions >1 cm in decubitus view
if suspect due to CHF, can diurese and see if effusions resolve (75% do so in 48 h)
asymmetry, fever
,
chest pain or failure to resolve
→ thoracentesis
parapneumonics should be tapped ASAP
(
cannot
exclude infxn clinically)
Diagnostic studies:
✓ total protein, LDH, glucose, cell count w/ differential, Gram stain & culture, pH; remaining fluid for additional studies as dictated by clinical scenario
Complications:
PTX (5–10%), hemothorax (~1%), re-expansion pulm edema (if >1.5 L removed), spleen/liver lac.; post-tap CXR not routinely needed (
Annals
1996;124:816)
↓ PTX w/ U/S and experienced supervisor (
Chest
2009;135:1315;
Archives
2010;170:332)
•
Transudate vs. exudate
(
Annals
1972;77:507)
Light’s criteria
: exudate = TP
eff
/TP
serum
>0.5
or
LDH
eff
/LDH
serum
>0.6
or
LDH
eff
>
2
/
3
ULN of LDH
serum
; 98% Se, 83% Sp; best Se of all methods (
Chest
1995;107:1604); however, will misidentify 25% of transudates as exudates; ∴ if clinically suspect transudate but meets criterion for exudate, confirm w/ test w/ higher Sp
exudative criteria w/ better Sp: serum-effusion alb gradient ≤1.2, Se 87%, Sp 92%; serum-effusion TP gradient ≤3.1, Se 84%, Sp 91%; chol
eff
>45 mg/dL
and
LDH
eff
>200, 90% Se, 98% Sp (no serum required)
CHF effusions:
TP may
↑
with diuresis or chronicity
→ “pseudoexudate”; alb gradient ≤1.2, chol
eff
>60 mg/dL (Se 54%, Sp 92%) or clin judgment to distinguish (
Chest
2002;122:1524)
•
Complicated vs. uncomplicated parapneumonic
(
Chest
1995;108:299)
complicated =Gram stain or culture
or
pH <7.2
or
glucose <60
complicated parapneumonic effusions usually require
drainage
to achieve resolution
empyema = frank pus, also needs drainage to achieve resolution
• Additional pleural fluid studies (
NEJM
2002;346:1971)
NT-proBNP ≥1,500 pg/mL has 91% Se & 93% Sp for CHF (
Am J Med
2004;116:417)
WBC & diff.: exudates tend to have ↑ WBC vs. transudates but nonspecific neutrophils → parapneumonic, PE, pancreatitis lymphocytes (>50%) → cancer, TB, rheumatologic eos (>10%) → blood, air, drug rxn, asbestos, paragonimiasis, Churg-Strauss, PE
RBC: Hct
eff
1–20% → cancer, PE, trauma; Hct
eff
/Hct
blood
>50% → hemothorax
AFB: yield in TB 0–10% w/ stain, 11–50% w/ culture, ~70% w/ pleural bx
adenosine deaminase (ADA): seen w/ granulomas, >70 suggests TB, <40 excludes TB
cytology: ideally ≥150 mL and at least 60 mL should be obtained (
Chest
2010;137:68)
glucose: <60 mg/dL → malignancy, infection, RA
amylase: seen in pancreatic disease and esophageal rupture (salivary amylase)
rheumatoid factor, C
H
50, ANA:
limited utility
in dx collagen vascular disease
triglycerides: >110 → chylothorax, 50–110 → ✓ lipoprotein analysis for chylomicrons
cholesterol: >60; seen in chronic effusions (eg, CHF, RA, old TB)
creatinine: effusion/serum ratio >1 → urinothorax
fibulin-3: ↑ plasma and/or effusion levels → mesothelioma (
NEJM
2012;367:1417)
• Chest CT; pleural biopsy; VATS
• Undiagnosed persistent pleural effusions (
Clin Chest Med
2006;27:309)
Transudative
: most commonly CHF or hepatic hydrothorax. ✓ s/s CHF or cirrhosis, NT-proBNP
eff
; consider intraperitoneal injection of technetium-99m sulfur colloid
Exudative
(ensure using Sp test listed above): most commonly malig, empyema, TB, PE. ✓ s/s malig, chest CT (I
+
), ADA or IFN-g release assay; consider thoracoscopy.
Treatment
• Symptomatic effusion: therapeutic thoracentesis, treat underlying disease process • Parapneumonic effusion (
Chest
2000;118:1158)
uncomplicated → antibiotics for pneumonia
>
1
/
2
hemithorax
or
complicated
or
empyema
→
tube thoracostomy
(otherwise risk of organization and subsequent need for surgical decortication)
loculated→ tube thoracostomy or VATS; intrapleural t-PA + DNase ↓ need for surgical referral (
NEJM
2011;365:518)
• Malignant effusion: serial thoracenteses vs. tube thoracostomy + pleurodesis (success rate ~80–90%) vs. indwelling pleural catheter (
JAMA
2012;307:2383); choice of pleurodesis agent (talc, bleo, doxy) controversial; systemic steroids & pH <7.2 a/w ↑ pleurodesis failure rate • TB effusions: effusion will often resolve spontaneously; however, treat Pt for active TB
• Hepatic hydrothorax
Rx: Δ pressure gradient (ie, ↓ ascitic fluid volume, NIPPV)
avoid chest tubes; prn thoracenteses, pleurodesis, TIPS or VATS closure of diaphragmatic defects if medical Rx fails; NIPPV for acute short-term management
Other books
Apex Hides the Hurt by Colson Whitehead
Murder at Whitehall by Amanda Carmack
Submitting Sarah (Montana Maiden Series Book 4) by Vanessa Vale
Stand the Storm by Breena Clarke
The Boy in the Lot by Ronald Malfi
The Dopefiend by JaQuavis Coleman
Darkness at Dawn by Elizabeth Jennings
Rafferty's Legacy by Jane Corrie
A Late Divorce by A. B. Yehoshua
Entranced By Him by Cassandra Harper