Ross & Wilson Anatomy and Physiology in Health and Illness (116 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

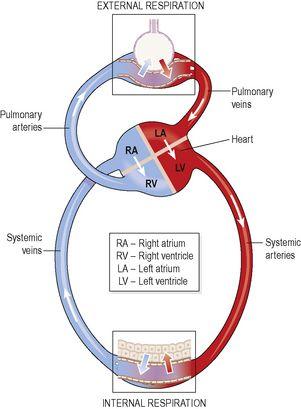
Figure 10.24
A.
External respiration.
B.
internal respiration.
Internal respiration
This is exchange of gases by diffusion between blood in the capillaries and the body cells. Gas exchange does not occur across the walls of the arteries carrying blood from the heart to the tissues, because their walls are too thick.
P
O
2
of blood arriving at the capillary bed is therefore the same as blood leaving the lungs. Blood arriving at the tissues has been cleansed of its CO
2
and saturated with O
2
during its passage through the lungs, and therefore has a higher
P
O
2
and a lower
P
CO
2
than the tissues. This creates concentration gradients between capillary blood and the tissues, and gas exchange therefore occurs (
Fig. 10.24B
). O
2
diffuses from the bloodstream through the capillary wall into the tissues. CO
2
diffuses from the cells into the extracellular fluid, then into the bloodstream towards the venous end of the capillary.
Figure 10.25
summarises the processes of internal and external respiration.
Figure 10.25
Summary of external and internal respiration.
Transport of gases in the bloodstream
Oxygen and carbon dioxide are carried in the blood in different ways.
Oxygen
Oxygen is carried in the blood in:
•
chemical combination with haemoglobin (see
Fig. 4.5, p. 59
) as
oxyhaemoglobin
(98.5%)
•
solution in plasma water (1.5%).
Oxyhaemoglobin is unstable, and under certain conditions readily dissociates releasing oxygen. Factors that increase dissociation include low O
2
levels, low pH and raised temperature (see
Ch. 4
). In active tissues there is increased production of carbon dioxide and heat, which leads to increased release of oxygen. In this way oxygen is available to tissues in greatest need. Whereas oxyhaemoglobin is bright red, deoxygenated blood is bluish-purple in colour.
Carbon dioxide
Carbon dioxide is one of the waste products of metabolism. It is excreted by the lungs and is transported by three mechanisms:
•
as bicarbonate ions (HCO
3
−
) in the plasma (70%)
•
some is carried in erythrocytes, loosely combined with haemoglobin as
carbaminohaemoglobin
(23%)
•
some is dissolved in the plasma (7%).
Regulation of air and blood flow in the lung
During quiet breathing, only a small portion of the lung’s total capacity is ventilated with each breath. This means that only a fraction of the total alveoli are being ventilated, usually in the upper lobes, and much of the remaining lung is temporarily collapsed. Airways supplying alveoli that are not being used are constricted, directing airflow into functioning alveoli. In addition, the pulmonary arterioles bringing blood into the ventilated alveoli are dilated, to maximise gas exchange, and blood flow (perfusion) past the non-functioning alveoli is reduced.
When respiratory requirements are increased, e.g. in exercise, the increased tidal volume expands additional alveoli, and the blood flow is redistributed to perfuse these too. In this way, air flow (ventilation) and blood flow (perfusion) are matched to maximise the opportunity for gas exchange.
Control of respiration
Effective control of respiration enables the body to regulate blood gas levels over a wide range of physiological, environmental and pathological conditions, and is normally involuntary. Voluntary control is exerted during activities such as speaking and singing but is overridden if blood CO
2
rises (hypercapnia).
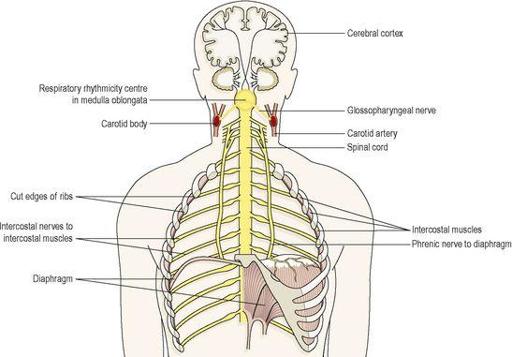
The respiratory centre
This is formed by groups of nerves in the medulla, the
respiratory rhythmicity centre
, which control the respiratory pattern, i.e. the rate and depth of breathing (
Fig. 10.26
). Regular discharge of
inspiratory neurones
within this centre set the rate and depth of breathing. Activity of the respiratory rhythmicity centre is adjusted by nerves in the pons (the
pneumotaxic centre
and the
apneustic centre
), in response to input from other parts of the brain.
Figure 10.26
Some of the structures involved in control of respiration.
Motor impulses leaving the respiratory centre pass in the
phrenic
and
intercostal nerves
to the diaphragm and intercostal muscles respectively.
Chemoreceptors
These are receptors that respond to changes in the partial pressures of oxygen and carbon dioxide in the blood and cerebrospinal fluid. They are located centrally and peripherally.
Central chemoreceptors
These are located on the surface of the medulla oblongata and are bathed in cerebrospinal fluid. When arterial
P
CO
2
rises (hypercapnia), even slightly, the central chemoreceptors respond by stimulating the respiratory centre, increasing ventilation of the lungs and reducing arterial
P
CO
2
. The sensitivity of the central chemoreceptors to raised arterial
P
CO
2
is the most important factor in controlling normal blood gas levels. A small reduction in
P
O
2
(hypoxaemia) has the same, but less pronounced effect, but a substantial reduction depresses breathing.
Peripheral chemoreceptors
These are situated in the arch of the aorta and in the carotid bodies (
Fig. 10.26
). They are more sensitive to small rises in arterial
P
CO
2
than to small decreases in arterial
P
O
2
levels. Nerve impulses, generated in the peripheral chemoreceptors, are conveyed by the
glossopharyngeal
and
vagus nerves
to the medulla and stimulate the respiratory centre. The rate and depth of breathing are then increased. An increase in blood acidity (decreased pH or raised [H
+
]) stimulates the peripheral chemoreceptors, resulting in increased ventilation, increased CO
2
excretion and increased blood pH.
Exercise and respiration
Physical exercise increases both the rate and depth of respiration to supply the increased oxygen requirements of the exercising muscles. Exercising muscles produces higher quantities of CO
2
, which stimulates central and peripheral chemoreceptors. The increased respiratory effort persists even after exercise stops, in order to supply enough oxygen to repay the ‘oxygen debt’. This represents mainly the oxygen needed to get rid of wastes, including lactic acid.
Other factors that influence respiration
Breathing may be modified by the higher centres in the brain by:
•
speech, singing
•
emotional displays, e.g. crying, laughing, fear
•
drugs, e.g. sedatives, alcohol
•
sleep.
Temperature influences breathing. In fever, respiration is increased due to increased metabolic rate, while in hypothermia it is depressed, as is metabolism. Temporary changes in respiration occur in swallowing, sneezing and coughing.
The
Hering–Breuer reflex
prevents overinflation of the lungs. Stretch receptors in the lung, linked to the respiratory centre by the vagus nerve, inhibit respiration when lung volume approaches maximum.
Disorders of the upper respiratory tract