Ross & Wilson Anatomy and Physiology in Health and Illness (115 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Inspiration
Simultaneous contraction of the external intercostal muscles and the diaphragm expands the thorax. As the parietal pleura is firmly adherent to the diaphragm and the inside of the ribcage, it is pulled outward along with them. This pulls the visceral pleura outwards too, since the two pleura are held together by the thin film of pleural fluid. Because the visceral pleura is firmly adherent to the lung, the lung tissue is, therefore, pulled up and out with the ribs, and downwards with the diaphragm. This expands the lungs, and the pressure within the alveoli and in the air passages falls, drawing air into the lungs in an attempt to equalise the atmospheric and alveolar air pressures.
The process of inspiration is
active
, as it needs energy for muscle contraction. The negative pressure created in the thoracic cavity aids venous return to the heart and is known as the
respiratory pump
.
At rest, inspiration lasts about 2 seconds.
Expiration
Relaxation of the external intercostal muscles and the diaphragm results in downward and inward movement of the ribcage (
Fig. 10.22
) and elastic recoil of the lungs. As this occurs, pressure inside the lungs rises and expels air from the respiratory tract. The lungs still contain some air, and are prevented from complete collapse by the intact pleura. This process is
passive
as it does not require the expenditure of energy.
At rest, expiration lasts about 3 seconds, and after expiration there is a pause before the next cycle begins.
Physiological variables affecting breathing
Elasticity
Elasticity is the term used to describe the ability of the lung to return to its normal shape after each breath. Loss of elasticity of the connective tissue in the lungs necessitates forced expiration and increased effort on inspiration.
Compliance
This is a measure of the stretchability of the lungs, i.e. the effort required to inflate the alveoli. The healthy lung is very compliant, and inflates with very little effort. When compliance is low the effort needed to inflate the lungs is greater than normal, e.g. in some diseases where elasticity is reduced or when insufficient surfactant is present. Note that compliance and elasticity are opposing forces.
Airway resistance
When this is increased, e.g. in bronchoconstriction, more respiratory effort is required to inflate the lungs.
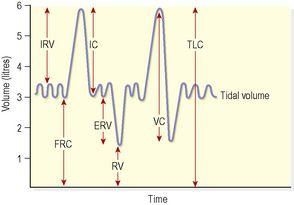
Lung volumes and capacities (
Fig. 10.23
)
In normal quiet breathing there are about 15 complete respiratory cycles per minute. The lungs and the air passages are never empty and, as the exchange of gases takes place only across the walls of the alveolar ducts and alveoli, the remaining capacity of the respiratory passages is called the
anatomical dead space
(about 150 ml).
Figure 10.23
Lung volumes and capacities.
IRV: inspiratory reserve volume; IC: inspiratory capacity; FRC: functional residual capacity; ERV: expiratory reserve volume; RV: residual volume; VC: vital capacity; TLC: total lung capacity.
Tidal volume (TV)
This is the amount of air passing into and out of the lungs during each cycle of breathing (about 500 ml at rest).
Inspiratory reserve volume (IRV)
This is the extra volume of air that can be inhaled into the lungs during maximal inspiration, i.e. over and above normal TV.
Inspiratory capacity (IC)
This is the amount of air that can be inspired with maximum effort. It consists of the tidal volume (500 ml) plus the inspiratory reserve volume.
Functional residual capacity (FRC)
This is the amount of air remaining in the air passages and alveoli at the end of quiet expiration. Tidal air mixes with this air, causing relatively small changes in the composition of alveolar air. As blood flows continuously through the pulmonary capillaries, this means that exchange of gases is not interrupted between breaths, preventing moment-to-moment changes in the concentration of blood gases. The functional residual volume also prevents collapse of the alveoli on expiration.
Expiratory reserve volume (ERV)
This is the largest volume of air which can be expelled from the lungs during maximal expiration.
Residual volume (RV)
This cannot be directly measured but is the volume of air remaining in the lungs after forced expiration.
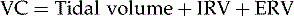
Vital capacity (VC)
This is the maximum volume of air which can be moved into and out of the lungs:
Total lung capacity (TLC)
This is the maximum amount of air the lungs can hold. In an adult of average build, it is normally around 6 litres. Total lung capacity represents the sum of the vital capacity and the residual volume. It cannot be directly measured in clinical tests because even after forced expiration, the residual volume of air still remains in the lungs.
Alveolar ventilation
This is the volume of air that moves into and out of the alveoli per minute. It is equal to the tidal volume minus the anatomical dead space, multiplied by the respiratory rate:
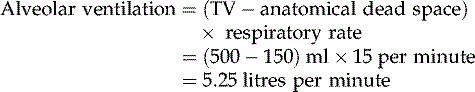
Lung function tests are carried out to determine respiratory function and are based on the parameters outlined above. Results of these tests can help in diagnosis and monitoring of respiratory disorders.
Exchange of gases
Although breathing involves the alternating processes of inspiration and expiration, gas exchange at the respiratory membrane and in the tissues is a continuous and ongoing process. Diffusion of oxygen and carbon dioxide depends on pressure differences, e.g. between atmospheric air and the blood, or blood and the tissues.
Composition of air
Atmospheric pressure at sea level is 101.3 kilopascals (kPa) or 760 mmHg. With increasing height above sea level, atmospheric pressure is progressively reduced and at 5500 m, about two-thirds the height of Mount Everest (8850 m), it is about half that at sea level. Under water, pressure increases by approximately 1 atmosphere per 10 m below sea level.
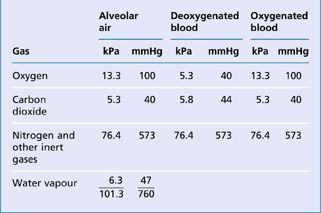
Air is a mixture of gases: nitrogen, oxygen, carbon dioxide, water vapour and small quantities of inert gases. The percentage of each in inspired and expired air is listed in
Table 10.1
. Each gas in the mixture exerts a part of the total pressure proportional to its concentration, i.e. the
partial pressure
(
Table 10.2
). This is denoted as, e.g.
P
O
2
,
P
CO
2
.
Table 10.1
The composition of inspired and expired air
| | Inspired air % | Expired air % |
|---|---|---|
| Oxygen | 21 | 16 |
| Carbon dioxide | 0.04 | 4 |
| Nitrogen and rare gases | 78 | 78 |
| Water vapour | Variable | Saturated |
Table 10.2
Partial pressures of gases
Alveolar air
The composition of alveolar air remains fairly constant and is different from atmospheric air. It is saturated with water vapour, and contains more carbon dioxide and less oxygen. Saturation with water vapour provides 6.3 kPa (47 mmHg) thus reducing the partial pressure of all the other gases present. Gaseous exchange between the alveoli and the bloodstream (
external respiration
) is a continuous process, as the alveoli are never empty, so it is independent of the respiratory cycle. During each inspiration only some of the alveolar gases are exchanged.
Diffusion of gases
Exchange of gases occurs when a difference in partial pressure exists across a semipermeable membrane. Gases move by diffusion from the higher concentration to the lower until equilibrium is established (
p. 25
). Atmospheric nitrogen is not used by the body so its partial pressure remains unchanged and is the same in inspired and expired air, alveolar air and in the blood.
External respiration
This is exchange of gases by diffusion between the alveoli and the blood in the alveolar capillaries, across the respiratory membrane. Each alveolar wall is one cell thick and is surrounded by a network of tiny capillaries (the walls of which are also only one cell thick). The total area of respiratory membrane for gas exchange in the lungs is about equivalent to the area of a tennis court. Venous blood arriving at the lungs has travelled from all the tissues of the body, and contains high levels of CO
2
and low levels of O
2
. Carbon dioxide diffuses from venous blood down its concentration gradient into the alveoli until equilibrium with alveolar air is reached. By the same process, oxygen diffuses from the alveoli into the blood. The relatively slow flow of blood through the capillaries increases the time available for gas exchange to occur. When blood leaves the alveolar capillaries, the oxygen and carbon dioxide concentrations are in equilibrium with those of alveolar air (
Fig. 10.24A
).