Ross & Wilson Anatomy and Physiology in Health and Illness (120 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

•
breakdown of capillary walls.
In severe cases pneumonia may develop, followed by pulmonary hypertension and right-sided heart failure.
Retinopathy of prematurity
This affects premature babies requiring high-concentration oxygen therapy. The oxygen may stimulate immature retinal blood vessels to constrict causing fibrosis, retinal detachment and blindness (
p. 205
).
Lung infections
Learning outcome
After studying this section, you should be able to:
describe the causes and effects of lung infection, including pneumonia, abscess and tuberculosis.
Pneumonia (
Fig. 10.30
)
Pneumonia means infection of the alveoli. This occurs when protective processes fail to prevent inhaled or blood-borne microbes reaching and colonising the lungs. The following are some predisposing factors.
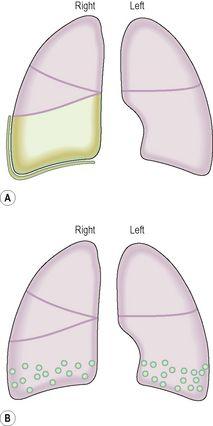
Figure 10.30
Distribution of infected tissue in: A.
Lobar pneumonia.
B.
Bronchopneumonia.
Impaired coughing
Coughing is an effective cleaning mechanism, but if it is impaired by, e.g., unconsciousness, damage to respiratory muscles or the nerves supplying them, or painful coughing, then respiratory secretions may accumulate and become infected.
Damage to the epithelial lining of the tract
Ciliary action may be impaired or the epithelium destroyed by, e.g., tobacco smoking, inhaling noxious gases, infection.
Impaired alveolar phagocytosis
Depressed macrophage activity may be caused by tobacco smoking, alcohol, anoxia, oxygen toxicity.
Other factors
The risk of pneumonia is increased in:
•
extremes of age
•
leukopenia
•
chronic disease, e.g. cardiac failure, cancer, chronic renal failure, alcoholism
•
suppression of immunity caused by, e.g., ionising radiation, corticosteroid drugs
•
hypothermia
•
mechanically assisted ventilation.
Causative organisms
A wide variety of organisms, including bacteria, viruses, mycoplasma, protozoa and fungi, can cause pneumonia under appropriate conditions. The commonest pathogen, especially in lobar pneumonia, is the bacterium
Streptococcus pneumoniae
. Others include
Staphylococcus aureus
and
Haemophilus influenzae
.
Box 10.1
lists other organisms sometimes responsible for pneumonia.
Box 10.1
Pathogens associated with pneumonia
| Mycoplasma |
| Legionella pneumonophilae |
| Klebsiella pneumoniae |
| Pseudomonas pyocyanea |
Lobar pneumonia (
Fig. 10.30A
)
This is infection of one or more lobes, usually by
Streptococcus pneumoniae
, leading to production of watery inflammatory exudate in the alveoli. This accumulates and fills the lobule which then overflows into and infects adjacent lobules. It is of sudden onset and pleuritic pain accompanies inflammation of the visceral pleura. If not treated by antibacterial drugs the disease goes through a series of stages followed by resolution and reinflation of the lobes in 2 to 3 weeks. This form of pneumonia is most common in previously healthy young adults.
Bronchopneumonia (
Fig. 10.30B
)
Infection spreads from the bronchi to terminal bronchioles and alveoli. As these become inflamed, fibrous exudate accumulates and there is an influx of leukocytes. Small foci of consolidation develop. There is frequently incomplete resolution with fibrosis. Bronchiectasis is a common complication leading to further acute attacks, lung fibrosis and progressive destruction of lung substance. Bronchopneumonia occurs most commonly in infancy and old age, and death is fairly common, especially when the condition complicates debilitating diseases. Predisposing factors include:
•
debility due to, e.g., cancer, uraemia, cerebral haemorrhage, congestive heart failure, malnutrition, hypothermia
•
lung disease, e.g., bronchiectasis, cystic fibrosis or acute viral infection
•
general anaesthetics, which depress respiratory and ciliary activity
•
inhalation of gastric contents (
aspiration pneumonia
) in, e.g., unconsciousness, very deep sleep, following excessive alcohol consumption, drug overdose
•
inhalation of infected material from the paranasal sinuses or upper respiratory tract.
Lung abscess
This is localised suppuration and necrosis within the lung substance.
Sources of infection
The abscess may develop from local infection:
•
if pneumonia is inadequately treated
•
as a result of trauma, e.g. rib fracture, stab wound or surgery
•
of adjacent structures, e.g. oesophagus, spine, pleural cavity, or a subphrenic abscess.
Occasionally a lung abscess develops when infected material travelling in the bloodstream, a
septic embolus
, arrives and lodges in the lung. Such material usually originates from a thrombophlebitis (
p. 113
) or infective endocarditis (
p. 121
).
Outcomes
Recovery from lung abscess may either be complete or lead to complications, e.g.:
•
chronic suppuration
•
septic emboli may spread to other parts of the body, e.g. the brain, causing cerebral abscess or meningitis
•
subpleural abscesses may spread and cause empyema and possibly bronchopleural fistula formation
•
erosion of a pulmonary blood vessel, leading to haemorrhage.
Tuberculosis (TB)
This infection is caused by one of two similar forms of mycobacteria, the main one being
Mycobacterium tuberculosis
. Humans are the main host. The microbes cause pulmonary tuberculosis and are spread either by droplet infection from an individual with active tuberculosis, or in dust contaminated by infected sputum. Less commonly in developed countries because of pasteurisation of milk, TB can be caused by
Mycobacterium bovis
, from cows.
Phases of pulmonary tuberculosis
Primary tuberculosis
When microbes are inhaled they colonise a lung bronchiole, usually towards the apex of the lung. There may be no evidence of clinical disease during the initial stage of non-specific inflammation. Later, cell-mediated T-lymphocytes respond to the microbes (antigens) and the individual becomes
sensitised
. Macrophages surround the microbes at the site of infection, forming
Ghon foci
(tubercles). These walled-off tubercles shelter microbes from normal body defences. Some macrophages containing live microbes are spread in lymph and infect hilar lymph nodes.
Primary complexes
are formed, consisting of
Ghon foci
plus infected hilar lymph nodes. Necrosis may reduce the core of foci to a cheese-like substance consisting of dead macrophages, dead lung tissue and live and dead microbes. Primary tuberculosis is usually asymptomatic. There are various outcomes.
•
The disease may be permanently arrested, the foci becoming fibrosed and calcified.
•
Microbes may survive in the foci and become the source of
secondary infection
months or years later.