Ross & Wilson Anatomy and Physiology in Health and Illness (114 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

compare the processes of internal and external respiration, using the concept of diffusion of gases
describe O
2
and CO
2
transport in the blood
explain the main mechanisms by which respiration is controlled.
The term respiration means the exchange of gases between body cells and the environment. This involves two main processes:
Breathing (pulmonary ventilation)
This is movement of air into and out of the lungs.
Exchange of gases
This takes place:
•
in the lungs:
external respiration
•
in the tissues:
internal respiration
.
Each of these will be considered later in this section.
Breathing
Breathing supplies oxygen to the alveoli, and eliminates carbon dioxide.
Muscles of breathing
Expansion of the chest during inspiration occurs as a result of muscular activity, partly voluntary and partly involuntary. The main muscles used in normal quiet breathing are the
external intercostal muscles
and the
diaphragm
.
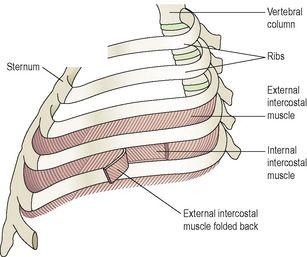
Intercostal muscles
There are 11 pairs of intercostal muscles that occupy the spaces between the 12 pairs of ribs. They are arranged in two layers, the external and internal intercostal muscles (
Fig. 10.20
).
Figure 10.20
The intercostal muscles and the bones of the thorax.
The external intercostal muscles
These extend downwards and forwards from the lower border of the rib above to the upper border of the rib below. They are involved in inspiration.
The internal intercostal muscles
These extend downwards and backwards from the lower border of the rib above to the upper border of the rib below, crossing the external intercostal muscle fibres at right angles. The internal intercostals are used when exhalation becomes active, as in exercise.
The first rib is fixed. Therefore, when the external intercostal muscles contract they pull all the other ribs towards the first rib. Because of the shape and sizes of the ribs they move outwards when pulled upwards, enlarging the thoracic cavity. The intercostal muscles are stimulated to contract by the
intercostal nerves
.
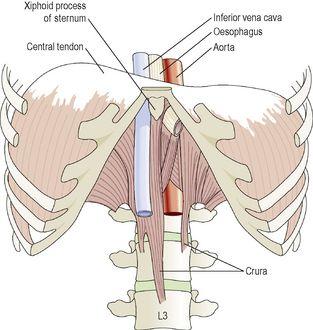
Diaphragm
The diaphragm is a dome-shaped muscular structure separating the thoracic and abdominal cavities. It forms the floor of the thoracic cavity and the roof of the abdominal cavity and consists of a central tendon from which muscle fibres radiate to be attached to the lower ribs and sternum and to the vertebral column by two crura. When the muscle of the diaphragm is relaxed, the central tendon is at the level of the 8th thoracic vertebra (
Fig. 10.21
). When it contracts, its muscle fibres shorten and the central tendon is pulled downwards to the level of the 9th thoracic vertebra, lengthening the thoracic cavity. This decreases pressure in the thoracic cavity and increases it in the abdominal and pelvic cavities. The diaphragm is supplied by the
phrenic nerves
.
Figure 10.21
The diaphragm.
Quiet, restful breathing is sometimes called
diaphragmatic breathing
because 75% of the work is done by the diaphragm.
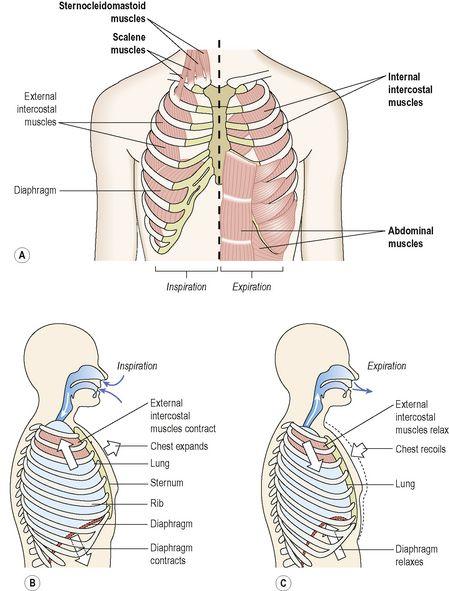
The external intercostal muscles and the diaphragm contract simultaneously, enlarging the thoracic cavity in all directions, that is from back to front, side to side and top to bottom (
Fig. 10.22
).
Figure 10.22
Changes in chest size during inspiration. A.
Muscles involved in respiration (accessory muscles labelled in bold).
B, C.
Changes in chest volume.
Accessory muscles of respiration
When extra respiratory effort is required, additional muscles are used. Forced inspiration is assisted by the
sternocleidomastoid
muscles (
p. 414
) and the
scalene
muscles, which link the cervical vertebrae to the first two ribs, and increase ribcage expansion. Forced expiration is helped by the activity of the internal intercostal muscles and sometimes the abdominal muscles, which increase the pressure in the thorax by squeezing the abdominal contents.
Cycle of breathing
The average respiratory rate is 12 to 15 breaths per minute. Each breath consists of three phases:
•
inspiration
•
expiration
•
pause.
As described previously, the visceral pleura is adherent to the lungs and the parietal pleura to the inner wall of the thorax and to the diaphragm. Between them is a thin film of serous fluid (
p. 243
).
Breathing is dependent upon changes in pressure and volume in the thoracic cavity. It follows the underlying physical principle that increasing the volume of a container decreases the pressure inside it, and that decreasing the volume of a container increases the pressure inside it. Since air flows from an area of high pressure to an area of low pressure, changing the pressure inside the lungs determines the direction of airflow.