Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (20 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
9.82Mb size Format: txt, pdf, ePub
Complications
•
Rupture
: pericardial sac → tamponade (avoid pericardiocentesis unless PEA); blood in pleural space, mediast., retroperitoneum; ↑ in hematoma on imaging portends rupture.
•
Malperfusion
(obstruction of branch artery)
can be
static
(avulsed/thrombosed) or
dynamic
(Δs in pressure in true vs. false lumen)
coronary → MI (usually RCA → IMI, since dissection often along outer Ao curvature)
innominate/carotid → CVA, Horner; intercostal/lumbar → spinal cord ischemia/paraplegia
innominate/subclavian → upper extremity ischemia; iliac → lower extremity ischemia
celiac/mesenteric → bowel ischemia; renal → acute renal failure, refractory HTN
•
AI
: due to annular dilatation or disruption or displacement of leaflet by false lumen • Mortality: 1–2%/h × 48 h for acute proximal; 10% at 30 d for acute distal
ARRHYTHMIAS
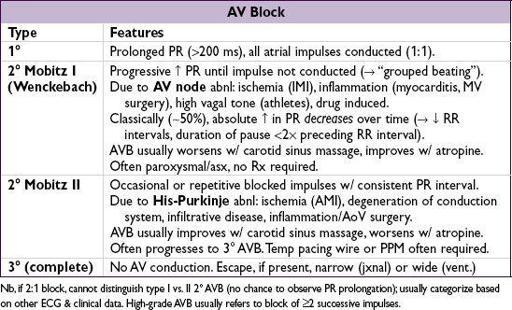
BRADYCARDIAS, AV BLOCK AND AV DISSOCIATION
Sinus bradycardia (SB) (
NEJM
2000;342:703)
• Etiologies:
meds
(incl bB, CCB, amio, Li, dig), ↑
vagal tone
(incl. athletes, sleep, IMI),
metabolic
(hypoxia, sepsis, myxedema, hypothermia, ↓ glc), OSA, ↑ ICP
• Treatment: usually none required; atropine, b
1
agonists or temp. pacing if symptomatic • Most common cause of sinus pause is
blocked premature atrial beat
Sick sinus syndrome (SSS)
• Features may include: periods of unprovoked SB, SA arrest, paroxysms of SB and atrial
tachyarrhythmias (“tachy-brady” syndrome), chronotropic incompetence w/ ETT
• Treatment: meds alone usually fail (adeq. control tachy → unacceptable brady); usually need
combination of meds
(bB, CCB, dig) for tachy &
PPM
for brady
AV dissociation
•
Default
: slowing of SA node allows subsidiary pacemaker (eg, AV junction) to take over •
Usurpation:
acceleration of subsidiary pacemaker (eg, AV junctional tach, VT) •
3
°
AV block:
atrial pacemaker unable to capture ventricles, subsidiary pacemaker emerges distinguish from
isorhythmic dissociation
(AV rate, some P waves nonconducting)
Temporary pacing wires
• Consider w/ bradycardia with hemodyn instability or unstable escape rhythm when perm pacer not readily available. Risks: RV perf, VT, PTX, CHB if existing LBBB,
etc.
• Consider instead of PPM for sx bradycardia due to reversible cause (bB/CCB O/D, Lyme, myocarditis, SBE, s/p cardiac surgery/trauma), TdP, acute MI (sx brady, high grade AVB)
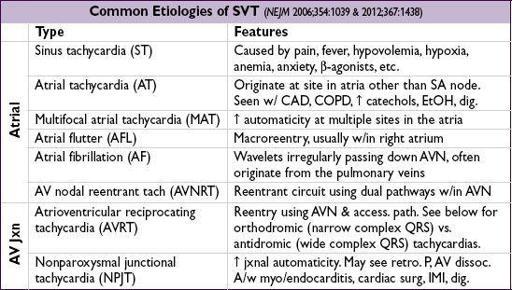
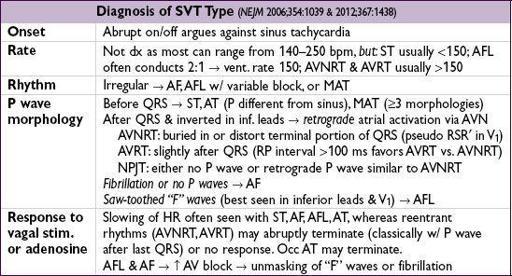
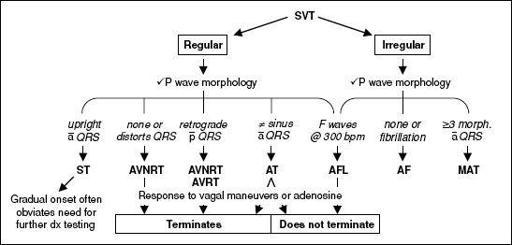
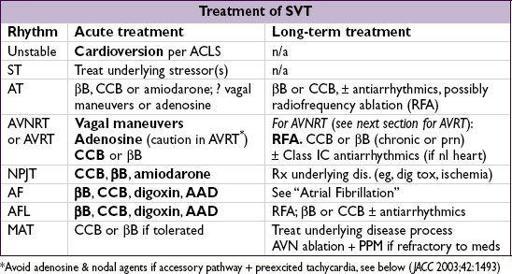
SUPRAVENTRICULAR TACHYCARDIAS (SVTS)
Arise above the ventricles
, ∴
narrow QRS
unless aberrant conduction or pre-excitation
.
Figure 1-4
Approach to SVT (adapted from
NEJM
2012;367:1438)
•
Catheter ablation
: high overall success rate (AFL/AVNRT ~95%, AVRT ~90%, AF ~80%)
Complications: stroke, MI, bleeding, perforation, conduction block (
JAMA
2007;290:2768)
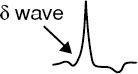
ACCESSORY PATHWAYS (WOLFF-PARKINSON-WHITE)
Definitions
•
Accessory pathway
(bypass tract) of conducting myocardium connecting atria & ventricles, allowing impulses to bypass normal AVN delay •
Preexcitation (WPW) pattern
: ↓ PR interval, ↑ QRS width w/ Δ wave (slurred onset,
can be subtle
), ST & Tw abnl (can mimic old IMI);
only seen w/ pathways that conduct antegrade
(if pathway only conducts retrograde then
ECG will be normal during SR; “concealed” bypass tract)
PAC can exaggerate preexcitation if AV node conduction slowed
•
WPW syndrome
: accessory pathway + paroxysmal tachycardia
Classic tachycardias of WPW
•
Orthodromic AVRT
:
narrow-complex
SVT (typically), conducting ↓ AVN & ↑ accessory pathway; requires retrograde conduction and ∴ can occur w/ concealed bypass tracts •
Antidromic AVRT
(rare):
wide-complex
SVT, conducting ↓ accessory pathway & ↑ AVN;
requires antegrade conduction and ∴ should see WPW pattern during SR
•
AF
w/ rapid conduction down accessory pathway; ∴ wide-complex irregular SVT; requires antegrade conduction; ∴ should see WPW pattern in SR. Rarely can degenerate into VF.
Treatment
•
AVRT
: vagal, bB, ? CCB; caution w/ adenosine (can precip. AF);
have defibrillator ready
•
AF/AFL
w/ conduction down accessory pathway: need to Rx arrhythmia
and
↑ pathway
refractoriness; use
procainamide
,
ibutilide
, amio, flecainide or DCCV; avoid CCB & bB (ineffective), dig/adenosine (can ↓ refractoriness of pathway → ↑ vent. rate → VF)
•
Long term
: Rx sx tachycardias w/ RFA, antiarrhythmics (IA, IC) if not candidate for RFA;
consider RFA if asx but AVRT or AF inducible on EPS (
NEJM
2003;349:1803) of if rapid conduction possible (✓ w/ EPS if preexcitation persists despite exercise testing)
risk of SCD related to how short RR interval is in AF and if SVT inducible w/ exercise
WIDE-COMPLEX TACHYCARDIAS (WCTS)
Etiologies (
Lancet
2012;380:1520)
•
Ventricular tachycardia (VT)
•
SVT conducted with aberrancy
: either fixed BBB, rate-dependent BBB (usually RBBB), conduction via an accessory pathway or atrially triggered ventricular pacing
Monomorphic ventricular tachycardia (MMVT)
Other books
Slaughter's way by Edson, John Thomas
Gaslight by Mark Dawson
Chalados y chamba by Marcus Sedgwick
Sarasota Sin by Scott, Talyn
T.J. and the Hat-trick by Theo Walcott
Doctor Who: The Seeds of Doom by Philip Hinchcliffe
31 - City of Fiends by Michael Jecks
Starting Over (Treading Water Trilogy) by Force, Marie
Fences in Breathing by Brossard, Nicole