Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (10 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.35Mb size Format: txt, pdf, ePub
• Failure of heart to pump blood forward at sufficient rate to meet metabolic demands of peripheral tissues, or ability to do so only at abnormally high cardiac filling pressures • Low output (↓ cardiac output) vs. high output (↑ stroke volume ± ↑ cardiac output) • Left-sided (pulmonary edema) vs. right-sided (↑ JVP, hepatomegaly, peripheral edema) • Backward (↑ filling pressures, congestion) vs. forward (impaired systemic perfusion) • Systolic (inability to expel sufficient blood) vs. diastolic (failure to relax and fill normally) • Reduced (HFrEF) vs. preserved (HFpEF) left ventricular ejection fraction • Some degree of systolic and diastolic dysfxn, may occur regardless of ejection fraction
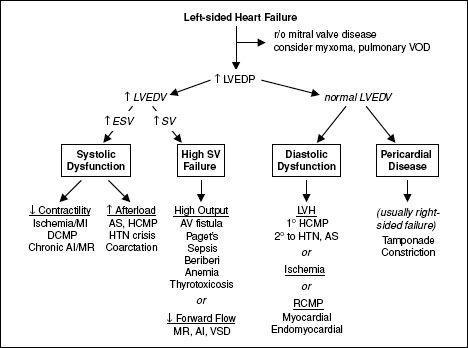
Figure 1-3
Approach to left-sided heart failure
History
• Low output: fatigue, weakness, exercise intolerance, Δ MS, anorexia • Congestive: left-sided → dyspnea, orthopnea, paroxysmal nocturnal dyspnea right-sided → peripheral edema, RUQ discomfort, bloating, satiety
Functional classification (New York Heart Association class)
• Class I: no sx w/ ordinary activity; class II: sx w/ ordinary activity; class III: sx w/ minimal activity; class IV: sx at rest
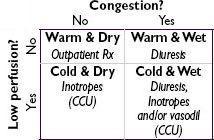
Physical exam (“2-minute” hemodynamic profile;
JAMA
1996;275:630 & 2002;287:628)
•
Congestion (“dry” vs. “wet”)
↑ JVP (~80% of the time JVP >10 → PCWP >22;
J Heart Lung Trans
1999;18:1126)
hepatojugular reflux: >4 cm ↑ in JVP for ≥15 sec w/ abdominal pressure Se/Sp 73/87% for RA >8 and Se/Sp 55/83% for PCWP >15 (
AJC
1990;66:1002)
Abnl Valsalva response: square wave (↑ SBP w/ strain), no overshoot (no ↑ BP after strain)
S
3
(in Pts w/ HF → ~40% ↑ risk of HF hosp. or pump failure death;
NEJM
2001;345:574)
rales, dullness at base 2° pleural effus. (
often absent
in chronic HF due to lymphatic compensation) ± hepatomegaly, ascites and jaundice, peripheral edema
•
Perfusion (“warm”
vs
. “cold”)
narrow pulse pressure (<25% of SBP) → CI <2.2 (91% Se, 83% Sp;
JAMA
1989;261:884)
soft S
1
(↓ dP/dt), pulsus alternans, cool & pale extremities, ↓ UOP, muscle atrophy
• ± Other: Cheyne-Stokes resp., abnl PMI (diffuse, sustained or lifting depending on cause of HF), S
4
(diast. dysfxn), murmur (valvular dis., ↑ MV annulus, displaced papillary muscles)
Evaluation for the presence of heart failure
• CXR (see Radiology insert): pulm edema, pleural effusions ± cardiomegaly, cephalization, Kerley B-lines • BNP/NT-proBNP can help exclude HF; levels ↑ w/ age, ↓ w/ obesity, ↓ renal fxn, AF
• Evidence of ↓ organ perfusion: ↑ Cr, ↓ Na, abnl LFTs • Echo (see inserts): ↓ EF & ↑ chamber size → systolic dysfxn; hypertrophy, abnl MV inflow, abnl tissue Doppler → ? diastolic dysfxn; abnl valves or pericardium; estimate RVSP
• PA catheterization: ↑ PCWP, ↓ CO and ↑ SVR (in low-output failure)
Evaluation of the causes of heart failure
• ECG: evidence for CAD, LVH, LAE, heart block or low voltage (? infiltrative CMP/DCMP) • Coronary angio (or noninvasive imaging, eg, CT angio); if no CAD, w/u for CMP
Precipitants of acute heart failure
•
Dietary indiscretion or medical nonadherence
(~40% of cases) •
Myocardial ischemia or infarction
(~10–15% of cases); myocarditis •
Renal failure
(acute, progression of CKD, or insufficient dialysis) → ↑ preload •
Hypertensive crisis (incl. from RAS)
,
worsening AS
→ ↑ left-sided afterload •
Drugs
(bB, CCB, NSAIDs, TZDs),
chemo
(anthracyclines, trastuzumab), or
toxins
(EtOH) • Arrhythmias; acute valvular dysfxn (eg, endocarditis), esp. mitral or aortic regurgitation • COPD or PE → ↑ right-sided afterload; anemia, systemic infection, thyroid disease
Treatment of acute decompensated heart failure
• Assess degree of congestion & adequacy of perfusion • For
congestion
:
“LMNOP”
L
asix IV w/ monitoring of UOP; total daily dose 2.5× usual daily PO dose → ↑ UOP, but transient ↑ in renal dysfxn vs. 1× usual dose; clear diff between cont gtt vs. q12h dosing (
NEJM
2011;364:797)
M
orphine (↓ sx, venodilator, ↓ afterload)
N
itrates (venodilator)
O
xygen ± noninvasive vent (↓ sx, ↑ P
a
O
2
; no ∆ mortality; see “Mechanical Ventilation”)
P
osition (sitting up & legs dangling over side of bed → ↓ preload)
• For
low perfusion
, see below • Adjustment of oral meds
ACEI/ARB: hold if HoTN, consider Δ to hydralazine & nitrates if renal decompensation
βB: reduce dose by at least ½ if mod HF, d/c if severe HF and/or need inotropes
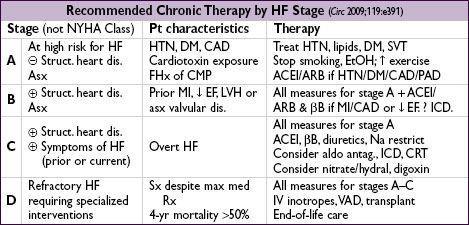
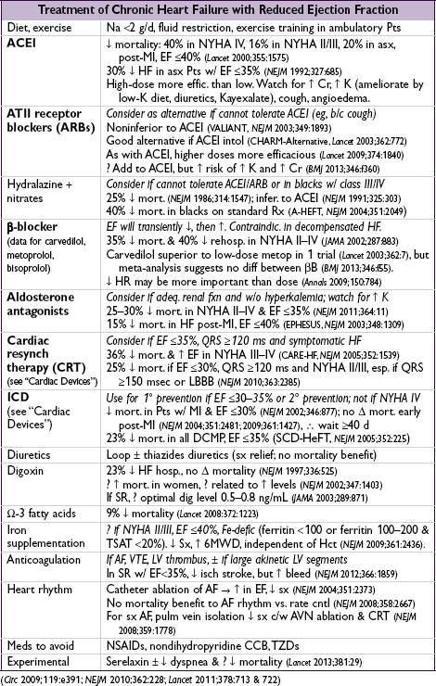
Treatment of advanced heart failure (
Circ
2009;119:e391)
• Consider PAC if not resp to Rx, unsure re: vol status, HoTN, ↑ Cr, need inotropes • Tailored Rx w/ PAC (qv); goals of MAP >60, CI >2.2 (MVO
2
>60%), SVR <800, PCWP <18
•
IV vasodilators
: NTG, nitroprusside (risk of coronary steal if CAD; prolonged use → cyanide/thiocyanate toxicity); nesiritide (rBNP) not rec for routine use (
NEJM
2011;365:32) •
Inotropes
(properties in addition to ↑ inotropy listed below)
dobutamine: vasodilation at doses ≤5 µg/kg/min; mild ↓ PVR; desensitization over time
dopamine: splanchnic vasodil. → ↑ GFR & natriuresis; vasoconstrictor at ≥5 µg/kg/min
milrinone: prominent systemic & pulmonary vasodilation; ↓ dose by 50% in renal failure
•
Ultrafiltration
: similar wt loss to aggressive diuresis, but ↑ renal failure (
NEJM
2012:367:2296) •
Mechanical circulatory support
(
Circ
2011;123:533)
Intra-aortic balloon pump (IABP): inflates in diastole & deflates in systole to ↓ impedance to LV ejection of blood, ↓ myocardial O
2
demand & ↑ coronary perfusion
ventricular assist device (LVAD ± RVAD): as bridge to recovery
(NEJM
2006;355:1873) or transplant (some temporary types can be placed percutaneously = PVAD), or as destination therapy (45–50% ↓ mort. vs. med Rx;
NEJM
2009;361:2241)
• Cardiac transplantation: 15–20% mort. in 1st y, median survival 10 y
• Utility of BNP-guided Rx remains debated (
Circ
2013;301:500 & 509) • Implantable PA pressure sensor in NYHA III → ~30% ↓ risk of hosp (
Lancet
2011;377:658)
Heart failure with preserved EF (HFpEF; “Diastolic HF”) (
Circ
2011;124:e540)
• Epidemiology: ~½ of Pts w/ HF have normal or only min. impaired systolic fxn (EF ≥40%); risk factors for HFpEF incl ↑ age,, DM, AF. Mortality
to those w/ systolic dysfxn.
Other books
Pumping Up Napoleon by Maria Donovan
Sunrise on the Mediterranean by Suzanne Frank
Sanctuary (Family Justice Book 3) by Halliday, Suzanne
Caroselli's Accidental Heir by Michelle Celmer
My Scandinavian Lover by Bella Donnis
Save Yourself by Kelly Braffet
Besieged by Bertrice Small
Fire on Dark Water by Perriman, Wendy
Your Body is Changing by Jack Pendarvis
The Clerk’s Tale by Margaret Frazer