Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (19 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.62Mb size Format: txt, pdf, ePub
•
Contrast CT
: quick, noninvasive, high Se & Sp for all aortic aneurysms •
TTE/TEE
: TTE most useful for root and proximal Ao; TEE can visualize other sites of TAA •
MRI
: preferred over CT for aortic root imaging for TAA; also useful in AAA but time-consuming; noncontrast “black blood” MR to assess aortic wall •
Abdominal U/S
: screening and surveillance test of choice for infrarenal AAA
Treatment (
Circ
2006;113:e463; 2008;177:1883; 2010;121:1544 & e266)
•
Risk factor modification
: smoking cessation, statin to achieve LDL-C <70 mg/dL
•
BP control
: b
B
(↓ dP/dt) ↓ aneurysm growth (
NEJM
1994;330:1335);
ACEI
a/w ↓ risk of rupture (
Lancet
2006;368:659),
ARB
may ↓ rate of aortic root growth in Marfan (
NEJM
2008;358:2787); no burst activity/exercise requiring Valsalva maneuvers (eg, heavy lifting) •
Indications for surgery
: individualize based on FHx, body size, gender
TAA
: sx; asc Ao ≥5.5 cm (? 5.0 cm Marfan, bicuspid AoV; 4.2–4.4 cm Loeys-Dietz); descending >6 cm; ↑ >0.5 cm/y; aneurysm ≥4.5 cm and planned AoV surgery
AAA
: infrarenal ≥5.5 cm (
NEJM
2002;346:1437) but consider ≥5.0 cm in; sx; ↑ >0.5 cm/y; inflam/infxn
•
Endovascular aneurysm repair
(EVAR) (
NEJM
2008;358:494;
Circ
2011;124:2020)
↓ short-term mort., bleeding, LOS; but long-term graft complic. (3–4%/y; endoleak, need for reintervention, rupture) necessitate periodic surveillance, with no proven Δ in overall mortality, except ? in those <70 y (
NEJM
2010;362:1863, 1881 & 2012;367:1988)
Guidelines support open repair or EVAR for infrarenal AAA in good surg candidates
In Pts unfit for surgery or high peri-op risks: ↓ aneurysm-related mortality but no Δ in overall mortality over medical Rx (
NEJM
2010;362:1872). EVAR noninferior (? superior) to open repair in ruptured AAA w/ favorable anatomy (
Ann Surg
2009;250:818).
TEVAR (thoracic EVAR) for descending TAA ≥5.5 cm may ↓ peri-op morbidity, no proven mortality benefit (
Circ
2010;121:2780;
JACC
2010;55:986;
J Thorac CV Surg
2010;140:1001)
Complications (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92)
•
Pain
: gnawing chest, back or abdominal pain; new or worse pain may signal rupture •
Rupture
: risk ↑ w/ diameter,, current smoking, HTN
TAA
: ~2.5%/y if <6 cm vs. 7%/y if >6 cm;
AAA
: ~1%/y if <5 cm vs. 6.5%/y if 5–5.9 cm
rupture p/w severe constant pain and hemorrhagic shock; ~80% mortality at 24 h
•
Acute aortic syndromes
(qv) •
Thromboembolic ischemic events
(eg, to CNS, viscera, extremities) •
Compression of adjacent structures
(eg, SVC, trachea, esophagus, laryngeal nerve)
Follow-up (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92; JAMA 2013;309:806)
• Expansion rate
0.1 cm/y for TAA,
0.3–0.4 cm/y for AAA • AAA: q3y if 3–3.9 cm; q6–12 mo if 4.0–5.4 cm (? q2y if 4–4.4) • TAA: 6 mo after dx to ensure stable, then annually.
• Screen for CAD, PAD and aneurysms elsewhere, esp. popliteal. About 25% of Pts w/
TAA will also have AAA, and 25% of AAA Pts will have a TAA: consider pan-Ao imaging.
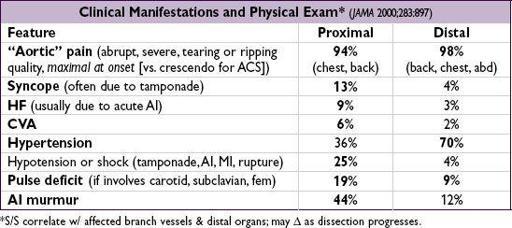
ACUTE AORTIC SYNDROMES
Definitions (
Circ
2003;108:628 & 2010;121:e266;
Eur Heart J
2012;33:26)
•
Aortic dissection
: intimal tear → blood extravasates into Ao media (creates false lumen) •
Intramural hematoma
(IMH): vasa vasorum rupture → medial hemorrhage that does not communicate with aortic lumen; 6% of aortic syndromes; clinically identical to AoD
•
Penetrating ulcer
: atherosclerotic plaque penetrates elastic lamina → medial hemorrhage
Classification (proximal twice as common as distal)
•
Proximal
: involves ascending Ao, regardless of origin (= Stanford A, DeBakey I & II) •
Distal
: involves descending Ao only, distal to L subclavian art. (= Stanford B, DeBakey III)
Risk factors
•
Hypertension
(h/o HTN in >70% of dissections);
male sex
(~70%); cocaine •
Connective tissue disease
:
Marfan
(fibrillin-1): arachnodactyly, joint disloc., pectus, ectopia lentis, MVP;
Ehlers-Danlos
type IV (type III procollagen): translucent skin; bowel or uterine rupture;
Loeys-Dietz
(TGFbR)
;
annuloaortic ectasia, familial AoD; PCKD
•
Congenital aortic anomaly
: bicuspid AoV, coarctation (eg, in Turner’s syndrome) •
Aortitis
(eg, Takayasu’s, GCA, Behçet’s, syphilis, now rare);
pregnancy
(typ. 3rd trim.) •
Trauma
: blunt, deceleration injury; IABP, cardiac or aortic surgery, cardiac catheterization
Diagnostic studies (
Circ
2005;112:3802; & 2010;121:e266;
Annals
2006;166:1350)
• Check bilateral BP and radial pulses for symmetry •
CXR
: abnl in 60–90% (↑ mediastinum, left pl effusion), but
cannot
be used to r/o dissection •
CT
: quick, noninvasive, readily available, Se ≥93% & Sp 98%; however, if& high clin. suspicion → additional studies (
2
⁄
3
w/ AoD have ≥2 studies;
AJC
2002;89:1235) •
TEE
: Se >95% prox, 80% for distal; can assess cors/peric/AI; “blind spot” behind trachea •
MRI
: Se & Sp >98%, but time-consuming test & not readily available •
Aortography
: Se ~90%, time-consuming, cannot detect IMH; can assess branch vessels •
D-dimer
: Se/NPV ~97%; ? <500 ng/mL to r/o dissec (
Circ
2009;119:2702); does not r/o IMH
Treatment (
Lancet
2008;372:55;
Circ
2010;121:1544;
JACC
2013;61:1661)
•
Initial Medical
: ↓
dP/dt
targeting HR ~60 & central BP 100–120 (or lowest that preserves perfusion; r/o pseudohypotension, eg, arm BP ↓ due to subclavian dissection)
first
with IV
b
B
(eg, propranolol, esmolol, labetalol) to blunt reflex ↑ HR & inotropy that would occur in response to vasodilators; verap/dilt if bB contraindic.
then
↓
SBP with IV vasodilators
(eg, nitroprusside)
control pain with MSO
4
prn to blunt sympathetic response
•
Proximal
: surgery (root replacement);
all acute
; chronic if c/b progression, AI or aneurysm •
Distal
: med Rx unless c/b progression, branch artery involvement → malperfusion/ ischemia, refractory HTN, refractory pain, rapid ↑ aneurysm size, rapid ↑ false lumen size. Repeat imaging: routinely (eg, 7 d, 3 wk, then q yr) & with any clinical or significant lab Δ. If complic., endovascular repair (covered stent graft to seal off entry, fenestrate flap, open occluded branch) preferred over surgery due to possible ↓ mort. (
JACC
2013;61:1661).
Other books
No Time for Goodbyes by Andaleeb Wajid
Everblue by Pandos, Brenda
The Laughing Gorilla by Robert Graysmith
Ivory Guard by Natalie Herzer
Gruffen by Chris D'Lacey
Blackout by Peter Jay Black
Porcelain Princess by Jon Jacks
Watch Over Me by Christa Parrish
A Virtuous Ruby by Piper Huguley