Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (80 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

PANCREATIC TUMORS
Pathology and genetics
(
Annu Rev Pathol
2008;3:157;
Nature
2012;491:399)
• Histologic types: adenocarcinoma, acinar cell carcinoma, endocrine tumors, cystic neoplasms (eg, IPMN, see below); rarely, mets to pancreas (eg, lung, breast, renal cell) • Pancreatic adenocarcinoma accounts for majority of pancreatic cancer (~85%) • Location: ~60% in head, 15% in body, 5% in tail; in 20% diffuse infiltration of pancreas • Mutations in adenoca.:
KRAS
(>90%),
p16
(80–95%),
p53
(50–75%),
SMAD4
(~55%)
Epidemiology and risk factors
(
Lancet
2011;378:607)
• Pancreatic adenocarcinoma 4th leading cause of cancer death in U.S. men and women • 80% of pancreatic adenocarcinomas occur in Pts 60–80 y • Acquired risk factors:
smoking
(RR ~1.5; 20% Pts), obesity, chronic pancreatitis, ? diabetes • Hereditary risk factors: genetic susceptibility may play a role in 5–10% of cases
Hereditary chronic pancreatitis: mutation in cationic trypsinogen gene (
PRSS1
)
Familial cancer syndromes and gene mutations with ↑ risk: familial atypical multiple mole melanoma (
CDKN2A/p16
), familial breast and ovarian cancer (
BRCA2
), Peutz-Jeghers (
LKB1
), ataxia-telangiectasia (
ATM
), ? hereditary colorectal cancer (HNPCC and FAP)
Clinical manifestations
•
Painless jaundice
(w/ pancreatic head mass),
pain
radiating to back, ↓
appetite & wt
• New-onset atypical diabetes mellitus (25%); unexplained malabsorption or pancreatitis • Migratory thrombophlebitis (Trousseau’s sign), not specific to panc cancer (
JCO
1986;4:509) • Exam: abd mass; nontender, palpable gallbladder (Courvoisier’s sign, but more often seen w/ biliary tract cancers); hepatomegaly; ascites; left supraclavicular (Virchow’s) node & palpable rectal shelf (both nonspecific signs of carcinomatosis) • Laboratory tests may show ↑ bilirubin, ↑ alk phos, anemia
Diagnostic and staging evaluation
(
NCCN Guidelines
v.2.2012)
•
Pancreatic protocol CT scan
(I
+
w/ arterial & venous phase imaging)
or MRI
• If no lesion seen → EUS, ERCP, MRI/MRCP may reveal mass or malignant ductal strictures • Biopsy pancreatic lesion via EUS-guided FNA (preferred in potential surgical candidates) or CT-guided (potential risk of seeding) or biopsy of possible metastasis • ↑ CA19-9 (nb, also ↑ in benign liver/biliary disease); may be useful to follow dis. postop
Treatment of pancreatic adenocarcinoma
(
NEJM
2010;362:1605;
Lancet
2011;378:607)
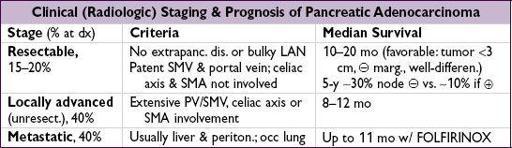
• Resectable: surgery ± adjuvant (neoadjuvant or postoperative) therapy
pancreaticoduodenectomy =
Whipple procedure
= resection of pancreatic head, duodenum, CBD and gallbladder ± partial gastrectomy
adjuvant therapy: ↑ survival but choice of regimen controversial (chemo vs. chemo/RT and gemcitabine vs. 5-FU (
J Surg Oncol
2013;107:78)
• Locally advanced: optimal strategy controversial. Gemcitabine alone vs. gemcitabine + RT (
JCO
2008;26:214s;
Ann Oncol
2008;19:1592;
JCO
2011;29:4105).
• Metastatic:
FOLFIRINOX
(5-FU + leucovorin, irinotecan, oxaliplatin) if good perform. status (
NEJM
2011;364:1817);
gemcitabine
combination (eg, w/ nab-paclitaxel;
JCO
2011;29:4548) or monotherapy if poor performance status (
JCO
1997;15:2403).
Offer clinical trials
.
• Palliative and supportive care:
obstructive jaundice or gastric outlet obstruction: endoscopic stenting or surgical bypass pain: opiates, celiac plexus neurolysis, radiation therapy weight loss: pancreatic enzyme replacement, nutrition consult, end-of-life discussions
Cystic lesions of the pancreas
(
NEJM
2004;351:1218;
Oncologist
2009;14:125)
• <10% of pancreatic neoplasms. Dx w/ CT, ERCP, MRCP or EUS.
•
Serous cystadenoma
: usually benign; central scar or honeycomb appearance on imaging •
Mucinous cystic neoplasm
(MCN): predominantly young females; multiloculated tumors in body or tail w/ ovarian-type stroma and mucin-rich fluid w/ ↑ CEA levels; precancerous •
Intraductal papillary mucinous neoplasm
(IPMN): neoplasm arising in main pancreatic duct or a branch; a/w ductal dilation w/ extrusion of mucinous material. Uncertain progression to cancer (? 5–20 y). Surgery based on age, size, location, dysplasia.
ONCOLOGIC EMERGENCIES
FEVER AND NEUTROPENIA (FN)
Definition
• Fever: single oral temp ≥38.3°C (101°F) or ≥38°C (100.4°F) for ≥1 h
•
Neutropenia:
ANC <500 cells/µL or <1000 cells/µL with predicted nadir <500 cells/µL
Pathophysiology and microbiology
• Predisposing factors: catheters, skin breakdown, GI mucositis, obstruction (lymphatics, biliary tract, GI, urinary tract), immune defect a/w malignancy
• Most episodes thought to result from seeding of bloodstream by GI flora
• Neutropenic enterocolitis (typhlitis): RLQ pain, watery/bloody diarrhea, cecal wall thickening
• GNRs (esp.
P. aeruginosa
) were historically most common
• Graminfections have recently become more common (60–70% of identified organisms)
• Fungal superinfection often results from prolonged neutropenia & antibiotic use
• Infection with atypical organisms and bacterial meningitis is rare
Prevention
• Levofloxacin (500 mg qd) ↓ febrile episodes & bacterial infections in chemo-related high-risk neutropenic patients; no difference in mortality (
NEJM
2005;353:977 & 988)
Diagnostic evaluation
• Exam: skin, oropharynx, lung, perirectal area, surgical & catheter sites; avoid DRE
• Labs: CBC with differential, electrolytes, BUN/Cr, LFTs, U/A
• Micro: blood (peripheral & through each indwelling catheter port), urine, & sputum cx; for localizing s/s → ✓ stool (
C. difficile
, cx), peritoneal fluid, CSF (rare source)
• Imaging: CXR; for localizing s/s → CNS, sinus, chest or abdomen/pelvis imaging
• Caveats: neutropenia → impaired inflammatory response →
exam and radiographic findings may be subtle
; absence of neutrophils by Gram stain does
not
r/o infection
Risk stratification
(factors that predict lower risk)
• History: age <60 y, no symptoms, no major comorbidities, cancer in remission, solid tumor, no h/o fungal infection or recent antifungal Rx
• Exam: temp <39°C, no tachypnea, no hypotension, no Δ MS, no dehydration
• Studies: ANC >100 cells/µL, anticipated duration of neutropenia <10 d, normal CXR
Initial antibiotic therapy
(
Clin Infect Dis
2011;52:e56)
• Empiric regimens including drug w/
antipseudomonal activity
; consider VRE coverage if colonized; OR 3.8 for VRE if VRE(
BBMT
2010;16:1576)
• PO abx may be used in low-risk Pts (<10 d neutropenia, nl hep/renal fxn, no N/V/D, no active infxn, stable exam): cipro + amoxicillin-clavulanate (
NEJM
1999;341:305)
• IV antibiotics: no clearly superior regimen; monotherapy or 2-drug regimens can be used
Monotherapy: ceftazidime, cefepime, imipenem or meropenem
2-drug therapy: aminoglycoside + antipseudomonal β-lactam
PCN-allergic: levofloxacin + aztreonam or aminoglycoside
•
Vancomycin
added in select cases (hypotension, indwelling catheter, severe mucositis, MRSA colonization, h/o quinolone prophylaxis), discontinue when cultures× 48 h
Modification to initial antibiotic regimen
• Low-risk Pts who become afebrile w/in 3–5 d can be switched to PO antibiotics
• Empiric antibiotics changed for fever >3–5 d or progressive disease (eg, add vancomycin)
• Antifungal therapy is added for neutropenic fever >5 d
liposomal amphotericin B, caspofungin, micafungin, anidulafungin, voriconazole, posaconazole all options (
NEJM
2002;346:225; 2007;356:348)
Duration of therapy
• Known source: complete standard course (eg, 14 d for bacteremia)