Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (101 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

• Discharge regimen: similar to admission regimen unless poor outPt cntl or strong reason for Δ. Arrange early insulin and glucometer teaching, prompt outPt follow-up.
DIABETIC KETOACIDOSIS (DKA)
Precipitants (the I’s)
•
Insulin defic.
(ie, failure to take enough insulin);
Iatrogenesis
(glucocorticoids) •
Infection
(pneumonia, UTI) or
Inflammation
(pancreatitis, cholecystitis) •
Ischemia
or
Infarction
(myocardial, cerebral, gut);
Intoxication
(alcohol, drugs)
Pathophysiology
• Occurs in
T1D
(and in ketosis-prone T2D); ↑ glucagon and ↓ insulin • Hyperglycemia due to: ↑ gluconeogenesis, ↑ glycogenolysis, ↓ glucose uptake into cells • Ketosis due to: insulin deficiency → mobilization and oxidation of fatty acids,
↑ substrate for ketogenesis, ↑ ketogenic state of the liver, ↓ ketone clearance
Clinical manifestations
(
Diabetes Care
2003;26:S109)
• Polyuria, polydipsia, & dehydration → ↑ HR, HoTN, dry mucous membranes, ↓ skin turgor • N/V, abdominal pain (either due to intra-abdominal process or DKA), ileus
• Kussmaul’s respirations (deep) to compensate for metabolic acidosis with odor of acetone • Δ MS → somnolence, stupor, coma; mortality ~1% even at tertiary care centers
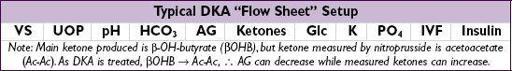
Diagnostic studies
• ↑
Anion gap metabolic acidosis
: can later develop nonanion gap acidosis due to urinary loss of ketones (HCO
3
equivalents) and fluid resuscitation with chloride •
Ketosis
:urine and serum ketones
(predominant ketone is β-OH-butyrate, but acetoacetate measured by assay; urine ketones may bein fasting normal Pts) • ↑ Serum glc; ↑ BUN & Cr (dehydration ± artifact due to ketones interfering w/ some assays) • Hyponatremia: corrected Na = measured Na + [2.4 × (measured glc −100)/100]
• ↓ or ↑ K (but even if serum K is elevated, usually
total body K depleted
); ↓ total body phos • Leukocytosis, ↑ amylase (even if no pancreatitis)
HYPEROSMOLAR HYPERGLYCEMIC STATE
Definition, precipitants, pathophysiology
(
Diabetes Care
2003;26:S33)
• Extreme hyperglycemia (w/o ketoacidosis) + hyperosm. + Δ MS in T2D (typically elderly) • Precip same as for DKA, but also include dehydration and renal failure • Hyperglycemia → osmotic diuresis → vol depletion → prerenal azotemia → ↑ glc,
etc.
Clinical manifestations & dx studies
(
Diabetes Care
2006;29[12]:2739)
• Volume depletion and Δ MS
• ↑
serum glc
(usually >600 mg/dL) and ↑
meas. serum osmolality
(>320 mOsm/L) effective Osm = 2 × Na (mEq/L) + glc (mg/dL)/18
• No ketoacidosis; usually ↑ BUN & Cr; [Na] depends on hyperglycemia & dehydration
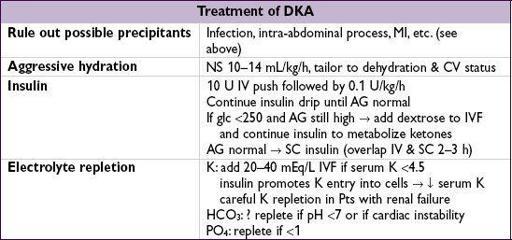
Treatment
(r/o possible precipitants; ~15% mortality due to precipitating factors)
•
Aggressive hydration
: initially NS, then
1
/
2
NS, average fluid loss up to 8–10 L
•
Insulin
(eg, 10 U IV followed by 0.05–0.1 U/kg/h)
HYPOGLYCEMIA
Clinical manifestations
(glucose <~55 mg/dL)
•
CNS
: headache, visual Δs, Δ MS, weakness, seizure, LOC (neuroglycopenic sx) •
Autonomic
: diaphoresis, palpitations, tremor (adrenergic sx)
Etiologies in diabetics
• Excess insulin, oral hypoglycemics, missed meals, renal failure (↓ insulin & SU clearance) • β-blockers can mask adrenergic symptoms of hypoglycemia
Etiologies in nondiabetics
• ↑
insulin
: exogenous insulin, sulfonylureas, insulinoma, anti-insulin antibodies • ↓
glucose production
: hypopituitarism, adrenal insufficiency, glucagon deficiency, hepatic failure, renal failure, CHF, alcoholism, sepsis, severe malnutrition • ↑
IGF-II
: non-islet tumor
• Postprandial, esp. postgastrectomy or gastric bypass: excessive response to glc load • Low glc w/o sx can be normal
Evaluation in nondiabetics
(
J Clin Endocrinol Metab
2009;94:709)
• If clinically ill: take measures to avoid recurrent hypoglycemia; ✓ BUN, Cr, LFTs, TFTs, prealbumin; IGF-I/IGF-II ratio when appropriate • If otherwise healthy: 72-h fast w/ monitored blood glc; stop for neuroglycopenic sx •
At time of hypoglycemia
: insulin, C peptide (↑ w/ insulinoma and sulfonylureas, ↓ w/ exogenous insulin), β-OH-butyrate, sulfonylurea levels • At end of fast, give 1 mg glucagon IV and measure response of plasma glc before feeding
Treatment
• Glucose tablets, paste, fruit juice are first-line Rx for Pts who can take POs • If IV access available, give 25–50 g of D
50
(50% dextrose) • If no IV, can give glucagon 0.5–1 mg IM or SC (side effect: N/V)
LIPID DISORDERS
Measurements
• Lipoproteins = lipids (cholesteryl esters & triglycerides) + phospholipids + proteins
include: chylomicrons, VLDL, IDL, LDL, HDL, Lp(a)
• Measure after 12-h fast; LDL is calculated = TC – HDL – (TG/5) (if TG >400, order
direct LDL measurement as calc. LDL inaccurate). Lipid levels stable up to 24 h
after ACS and other acute illnesses, then ↓ and may take 6 wk to return to nl.
• Metabolic syndrome (≥3 of following): waist ≥40” () or ≥35” (
); TG ≥150; HDL <40 mg/dL (
) or <50 mg/dL (
); BP ≥130/85 mmHg; fasting glc ≥100 mg/dL (
Circ
2009;120:1640)