Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (120 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
7.18Mb size Format: txt, pdf, ePub
•
Migraine
:
see below
Secondary causes of headaches
• Traumatic: postconcussion, SAH, SDH, postcraniotomy • ↑ ICP: mass (tumor, abscess, vascular malformations, ICH), hydrocephalus, idiopathic intracranial hypertension (pseudotumor cerebri), altitude associated cerebral edema • ↓ ICP: post-LP headache, CSF leak/dural tear, overshunting • Vascular causes: stroke (esp. posterior circ), dissection, vasculitis (incl. temporal arteritis), reversible cerebral vasoconstriction syndrome (RCVS), ICH, venous sinus thrombosis • Meningeal irritation: meningitis, SAH
• Trigeminal neuralgia • Extracranial: sinusitis, TMJ syndrome, glaucoma • Systemic causes: hypoxia, hypercapnia, dialysis HA, HTN, hypoglycemia, ↓TSH
• Medication overuse (analgesics), withdrawal (caffeine, opioids, estrogen)
Clinical evaluation (
JAMA
2006;296:1274)
• History: onset (sudden vs. gradual), quality, severity, location, duration, triggers, alleviating factors, positional component, hormonal triggers (menstruation), preceding trauma, associated sx (visual Δs, “floaters,” N/V, photophobia, focal neurologic sx) • Medications (analgesics), substance abuse (opioids, caffeine) • General and neurologic exam (fundoscopic exam, visual fields) •
Warning signs (should prompt neuroimaging)
explosive onset
(vasc);
“worst HA of my life”
(SAH, RCVS);
meningismus
(SAH, infxn)
positional
: lying > standing (↑ ICP);
N/V
(↑ ICP; migraines)
visual sx
: diplopia, blurring, ↓ acuity (GCA, glaucoma, ↑ ICP);
eye pain
(glaucoma, cluster)
abnl neuro exam
(struct. lesion, poss. in migraine); ↓
consciousness
(± fever): infxn, ICH
age
>
50 y
;
immunosuppression
(CNS infections, PRES)
• LP if suspicious for SAH (✓ for xanthochromia), pseudotumor (✓opening press); image first!
MIGRAINE
Epidemiology:
affects 15% of women and 6% of men; onset usually by 30 y
Definition & clinical manifestations (
Lancet
2004;363:381;
JAMA
2006;296:1274)
• H/o ≥5 attacks lasting 4–72 h and with (a) N/V
or
photophobia & phonophobia, and (b) ≥2 of following: unilat., pulsating, mod–severe intensity, aggravated by routine activity • Migraine w/o aura (64%): most common, previously called “common” migraine • Typical aura w/ migraine (18%): visual aura (scotomata with jagged/colored edge) precedes HA, can also be reversible sensory or speech symptoms, <1 h • Complicated: accompanied by stereotypical neurologic deficit that may last hrs (DDx includes
stroke
: in migraine onset is rather gradual, sx spread over mins) • Precipitants: stress, hunger, foods (cheese, chocolate) and food additives (MSG), fatigue, alcohol, menstruation, exercise
Treatment (
NEJM
2002;346:257)
• Eliminate precipitants
• Prophylaxis: TCA, βB, CCB, valproic acid, topiramate (
JAMA
2004;291:965), gabapentin • Abortive therapy: ASA, acetaminophen, caffeine, high-dose NSAIDs
metoclopramide IV, prochlorperazine IM or IV, valproate IV, steroids
5-HT
1
agonists (“triptans”): most specific therapy, contraindicated if complicated migraine, CAD, prior stroke. Triptan + NSAID stronger than either alone (
JAMA
2007;297:1443)
ergotamine, dihydroergotamine: use with caution in Pts w/ CAD
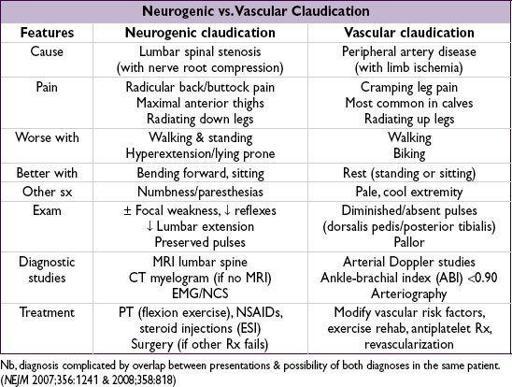
BACK AND SPINAL CORD DISEASE
Differential diagnosis of back pain
•
Musculoskeletal
: musculoligamentous “strain” (experienced by up to 80% of population at some time), OA, RA, spondylolisthesis, vertebral fx, inflammatory spondyloarthritis (ankylosing spondylitis, reactive, psoriatic), myofascial pain syndrome •
Spinal cord
(myelopathy)
/nerve root
(radiculopathy):
Degenerative/traumatic: disc herniation, spondylosis, vertebral fx and subluxation
Neoplastic: lung, breast, prostate, RCC, thyroid, colon, multiple myeloma, lymphoma
Infectious (also see ID section): osteomyelitis, epidural abscess, zoster, Lyme, CMV, HIV
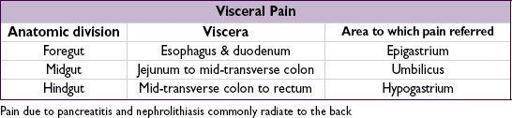
•
Referred pain from visceral disease
: (quality of pain can be important to distinguish)
GI: PUD, cholelithiasis, pancreatitis, pancreatic cancer
GU: pyelonephritis, nephrolithiasis, uterine or ovarian cancer, salpingitis
Vascular: aortic dissection, leaking aortic aneurysm
Initial evaluation
•
History
: location, radiation, trauma, wt loss, cancer hx, fever, immunocompromised, neurologic symptoms, saddle anesthesia, incontinence, urinary retention, IV drug use •
General physical exam
: local tenderness, ROM, signs of infection or malignancy,
signs of radiculopathy (experienced as sharp/lancinating pain radiating into limb):
Spurling sign (radicular pain w/ downward force to extended & ipsilaterally rotated head): 30% Se, 93% Sp
straight leg raise (radicular pain at 30–70°): ipsilateral: 92% Se, 28% Sp; crossed (contralateral leg raised): 28% Se, 90% Sp
•
Neurologic exam
: full motor (including sphincter tone), sensory (including perineal region) and reflexes including anal (S4) and cremasteric (L2) •
Laboratory
(depending on suspicion): CBC, ESR, Ca, PO
4
, AФ, CSF
•
Neuroimaging
: low yield if nonradiating pain, high falserate (incidental spondylosis) depending on suspicion: X-rays, CT or CT myelography, MRI, bone scan •
EMG/NCS
: may be useful to distinguish root/plexopathies from peripheral neuropathies
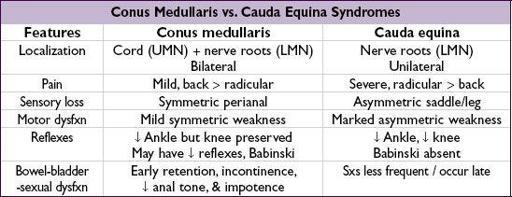
SPINAL CORD COMPRESSION
Clinical manifestations
• Acute: flaccid paraparesis and absent reflexes (“spinal shock”) • Subacute–chronic: spastic paraparesis and hyperactive reflexes • Posterior column dysfunction in legs (loss of vibratory sense or proprioception) • Sensory loss below level of lesion
• Bilateral prominent Babinski responses ± ankle clonus
Evaluation & treatment
• Empiric spine immobilization (collar, board) for all trauma patients • STAT MRI (at and above clinical spinal level, pre-and postgadolinium) or CT myelogram • Emergent neurosurgical and/or neurology consultation • Urgent radiation therapy ± surgery for compression if due to metastatic disease • High-dose steroids depending on cause:
Tumor: dexamethasone 16 mg/d IV (usually 4 mg q6h) with slow taper over wks
Trauma: methylprednisolone 30 mg/kg IV over 15 min then 5.4 mg/kg/h × 24 h (if started w/in 3 h of injury) or × 48 h (if started 3–8 h after injury) (
JAMA
1997;277:1597)
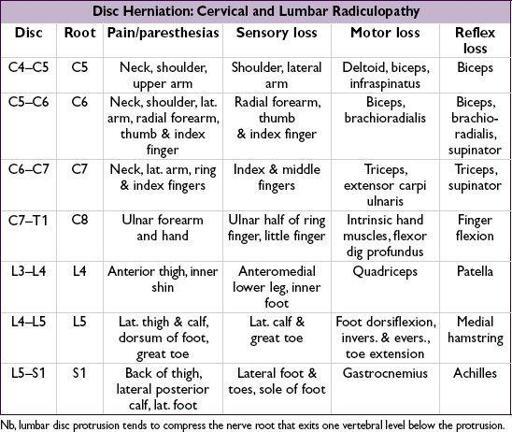
NERVE ROOT COMPRESSION
Clinical manifestations
• Radicular pain aggravated by activity (esp. bending, straining, coughing), relieved by lying • Sciatica = radicular pain radiating from buttocks down lateral aspect of leg, often to knee or lateral calf ± numbness and paresthesias radiating to lateral foot
Treatment of nerve root compression
• Conservative: avoid bending/lifting; NSAIDs; Rx neuropathic pain (see “Peripheral Neuropathies”); physical therapy • Spinal epidural steroid injections (ESI): limited short-term relief of refractory radicular pain • Surgery: cord compression or cauda equina syndrome; progressive motor dysfunction; bowel/bladder dysfunction; failure to respond to conservative Rx (
NEJM
2007;356:2245)
SURGICAL ISSUES
ABDOMINAL PAIN
Other books
A Pinstriped Finger's My Only Friend by Robert T. Jeschonek
One Bright Star to Guide Them by John C. Wright
Burning for You by Dunaway, Michele
Raging Sea by Michael Buckley
Death Takes a Gander by Goff, Christine
Ashenden by W. Somerset Maugham
Unfinished Business by Brenda Jackson
Assignment - Cong Hai Kill by Edward S. Aarons
Connect the Stars by Marisa de los Santos
Divide and Conquer by Carrie Ryan