Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (105 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

(
Lancet
2004;363:1277; NEJM 2004;350:1093;
Ann Rheum
Dis 2012;71:1448)
Clinical manifestations
• 4 stages: asx ↑ UA → acute gouty arthritis → intercritical (in between acute flares, usually asx) → chronic gouty arthropathy/tophaceous gout •
Asx hyperuricemia
: majority never develop gout •
Acute arthritis
: sudden onset (freq. nocturnal) of painful monoarticular arthritis
MTP of great toe (
podagra
); LE > UE; occasionally polyarticular (esp. in subseq flares)
precipitants: rapid Δ UA; ↑ dietary purine; surgery; infection; dehydration, meds (diuretics, urate lowering agents); ∴ frequent in hospitalized Pts
self-limited in 3–10 d; can involve bursa (eg, olecranon or patella); can mimic cellulitis
•
Intercritical period
: may be years but progressively shorter as freq of attacks ↑
•
Chronic tophaceous gout
: solid MSU crystal deposition in tissue & joints; commonly in joints (fingers, wrists, knees), pinna, Achilles tendon and pressure areas;
chronic gouty arthropathy
: deforming arthritis from tophus → pain, joint erosion
•
Renal
: uric acid stones; urate nephropathy (interstitial deposits)
Diagnostic studies
• ↑ UA does not make dx: 25% of measurements nl during flare; ± ↑ WBC & ESR
• Arthrocentesis: polarized microscopy →
needle-shaped
,
negatively
birefringent crystals
(yellow parallel to axis marked on polarizer), intracellular or extracellular (less specific)
WBC 20,000–100,000/mm
3
, >50% polys
infxn can coexist with acute attacks, ∴ always ✓ Gram stain & Cx (J Rheum 2012;39:157)
• Radiology: erosions with overhanging edge (late), useful to exclude chondrocalcinosis
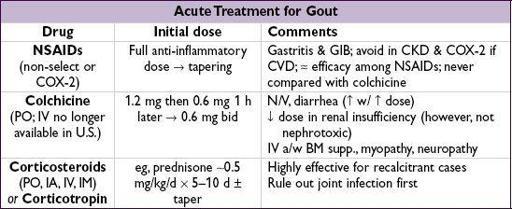
Acute treatment
(
Arthritis Care Res
2012;64:1447)
• No superior option; start w/in 24 h of sx onset; continue until acute flare resolves; for severe cases, consider combination therapy; rest and ice
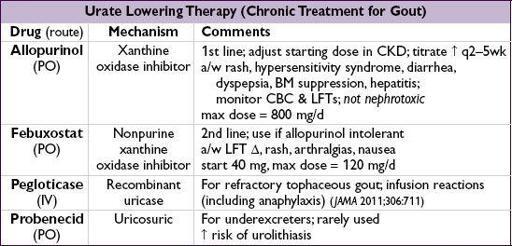
Chronic treatment
(
Lancet
2011;377:165)
•
Approach
: if ≥2 attacks/y, ≥1 tophus, joint erosions or urolithiasis → start urate lowering Rx & pharmacologic prophylaxis to ↓ risk of acute attacks •
Urate lowering Rx
: goal UA <6 mg/dL; do NOT discontinue during acute attack •
Pharmacologic prophylaxis
: continue for at least 6 mo or longer if frequent attacks:
low-dose
colchicine
(~50% ↓ risk of acute flare; J Rheum 2004;31:2429),
NSAIDs
(less evidence; Ann Rheum Dis 2006;65:1312), low-dose (<10 mg/d)
steroids
(min evidence)
•
Lifestyle
Δs: ↓ intake of meat, EtOH & seafood; ↑ low-fat dairy products; wt loss; avoid dehydration and hyperuricemia-promoting drugs (eg, diuretics)
•
Allopurinol hypersensitivity syndrome
: 10–25% mortality; ↓ risk by starting w/ dose 100 mg/d if eGFR >40 or 50 mg/d if eGFR <40; titrate up by 100 mg/d (if eGFR >40) or 50 mg/d (if eGFR <40) q2–5wk until goal UA (<6 mg/dL) reached (dose can be >300 mg/d even in CKD) (Arthritis Rheum 2012;64:2529; Arthritis Care Res 2012;64:1431)
CALCIUM PYROPHOSPHATE DIHYDRATE (CPPD) DEPOSITION DISEASE
Definition
• Deposition of CPPD crystals w/in tendons, ligaments, articular capsules, synovium, cartilage; frequently asymptomatic
Etiologies
(
Rheumatology
2012;51:2070)
• Most cases
idiopathic
; consider further metabolic eval in young (<50 y) and florid forms • Metabolic (3 H’s): hemochromatosis; hyperparathyroidism; hypomagnesemia (esp. in Gitelman’s or Bartter’s syndromes) • Joint trauma (incl. previous surgery); intra-articular hyaluronate can precipitate attacks • Familial chondrocalcinosis (autosomal dominant disorder); early-onset, polyarticular dis.
Clinical manifestations
(
Rheumatology
2009;48:711)
•
Chondrocalcinosis
: calcification of cartilage, resulting from CPPD deposition in articular cartilage, fibrocartilage or menisci.
↑ incidence w/ age; 20% >60 y have knee chondrocalcinosis in autopsy studies
• Pseudogout: acute CPPD crystal-induced mono-or asymmetric oligoarticular arthritis, indistinguishable from gout except through synovial fluid exam for crystals
location:
knees
,
wrists
and MCP joints
precipitants: surgery, trauma or severe illness
• “Pseudo-RA”: chronic polyarticular arthritis with morning stiffness • Pyrophosphate arthropathy: resembles OA and difficult to distinguish; may involve axial skeleton
Diagnostic studies
• Arthrocentesis
polarized microscopy →
rhomboid-shaped, weakly
positively
birefringent crystals
(yellow
perpendicular
and blue parallel to axis marked on polarizer)
WBC 2000–100,000/mm
3
,
>50% polys
infection can coexist with acute attacks, ∴ always ✓ Gram stain & Cx
• Screen for associated disease if young or severe: ✓ Ca, Mg, Fe, ferritin, TIBC, UA, PTH
•
Radiographs
: chondrocalcinosis appears as punctate and linear densities in articular cartilage, menisci, triangular fibrocartilage of wrist, small joints of fingers and symphysis pubis; may be asx (15% in Pts >60 y, 30–60% in Pts >80 y)
not a prerequisite for the diagnosis of CPPD disease
Treatment
(
Ann Rheum Dis
2011;70:571)
• Asymptomatic chondrocalcinosis requires no treatment • Acute therapy for pseudogout: no RCTs, extrapolated from practice in gout; ∴same as for gout, though colchicine not as effective • If associated metabolic disease, Rx of underlying disorder may improve arthritis sx • Low-dose daily colchicine or NSAID may be effective for prophylaxis or chronic arthropathy
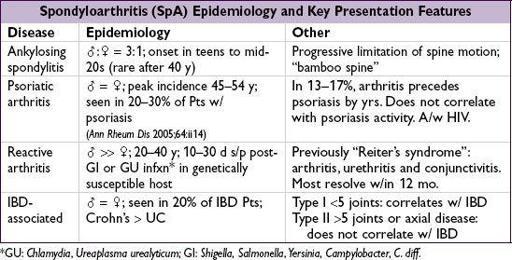
SERONEGATIVE SPONDYLOARTHRITIS
Classification system
(
Curr Opin Rheumatol 2010;22:375)
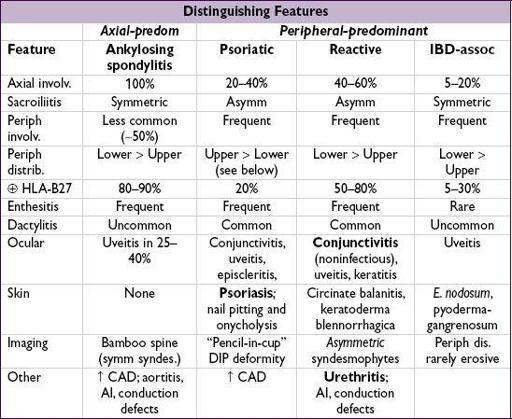
• 5 subtypes: ankylosing spondylitis (most common), reactive arthritis, psoriatic arthritis, IBD-associated arthritis and undifferentiated • All subtypes share common clinical manifestations: inflammatory spine disease, peripheral arthritis, enthesitis and extra-articular manifestations (primarily ocular and skin disease)
Epidemiology & pathogenesis
(
Semin Arthritis Rheum
2008;38:83)
• ↑ prevalence of HLA-B27; HLA-B27 accounts for ~30% of attributable genetic risk • Environmental factors likely critical for disease, esp. reactive arthritis (eg, infection) • Prevalence of 0.5–2% of population, worldwide
Major clinical manifestations
(
Lancet
2011;377:2127)
•
Inflammatory back pain
: SI joints (
sacroiliitis
), apophyseal joints of spine
characterized by
IPAIN
(
I
nsidious onset,
P
ain at night,
A
ge of onset <40 y,
I
mproves w/ exercise/hot water,
N
o improvement w/ rest), a.m. stiffness,
responsive to NSAIDs
•
Peripheral arthritis
: typically asymmetric, oligoarticular, large joints, lower > upper limb; however, can be symmetric & polyarticular (thus, mimic RA), esp. in psoriatic arthritis •
Enthesitis
: inflammation at site of tendon/ligament insertion into bone, esp. Achilles, pre-patellar, elbow epicondyles, plantar fasciitis.
Rigidity of spine
(bamboo spine by X-ray, ankylosis due to progressive growth of bony spurs which bridge intervertebral disc).
•
Dactylitis
(“sausage digit”): inflammation of entire digit (joint + tenosynovial inflamm) •
Uveitis
: anterior uveitis most common extra-articular manifestation; p/w pain, red eye, blurry vision, photophobia, usually unilateral