Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (100 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

• Rickets and/or osteomalacia: chronic ↓ vit Δ → ↓ Ca, ↓ PO
4
→ ↓ bone/cartilage mineralization, growth failure, bone pain, muscle weakness •
Renal osteodystrophy
(↓ vit Δ & ↑ PTH in renal failure): osteomalacia [↓ mineralization of bone due to ↓ Ca and 1,25-(OH)
2
D] & osteitis fibrosa cystica (due to ↑ PTH)
Diagnostic studies
• Ca, alb, ICa, PTH, 25-(OH)D, 1,25-(OH)
2
D (if renal failure or rickets), Cr, Mg, PO
4
, Af, U
Ca
Treatment
(also treat concomitant vitamin Δ deficiency)
• Symptomatic: Ca gluconate (1–2 g IV over 20 mins) + calcitriol (most effective in acute hypocalcemia, but takes hrs to work) ± Mg (50–100 mEq/d) • Asymptomatic and/or chronic: oral Ca (1–3 g/d; Ca citrate better absorbed then Ca carbonate, esp. if on PPI) & vitamin Δ (eg, ergocalciferol 50,000 IU PO q wk × 8–10 wk). In chronic hypopara., calcitriol is needed, consider also thiazide.
• Chronic renal failure: phosphate binder(s), oral Ca, calcitriol or analogue (calcimimetic may be needed later to prevent hypercalcemia)
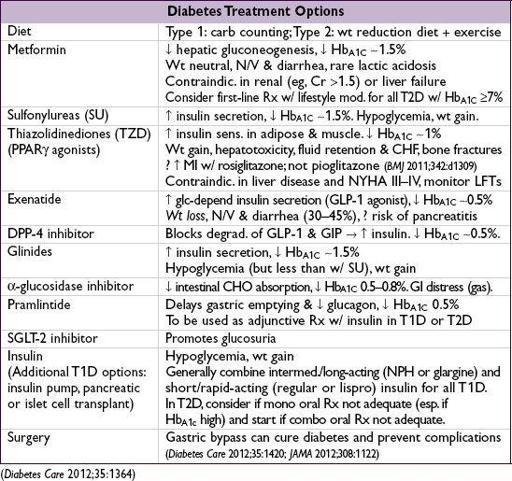
DIABETES MELLITUS
Definition
(
Diabetes Care
2010;33:S62;
NEJM
2012;367:542)
• Hb
A1c
≥6.5
or
fasting glc ≥126 mg/dL × 2
or
random glc ≥200 mg/dL × 2 (× 1 if severe hyperglycemia and acute metabolic decomp); routine OGTT not recommended (except during pregnancy) • Blood glc higher than normal, but not frank DM (“prediabetics,” ~40% U.S. population)
Hb
A1c
5.7–6.4%
or
impaired fasting glc (IFG): 100–125 mg/dL
Preventing progression to DM: diet & exercise (58% ↓), metformin (31% ↓;
NEJM
2002;346:393), TZD (60% ↓;
Lancet
2006;368:1096)
Categories
•
Type 1
: islet cell destruction; absolute insulin deficiency; ketosis in absence of insulin; prevalence 0.4%; usual onset in childhood but can occur throughout adulthood; ↑ risk ifFHx; HLA associations; anti-GAD, anti-islet cell & anti-insulin autoAb •
Type 2
: insulin resistance + relative insulin ↓; prevalence 8%; onset generally later in life; no HLA associations; risk factors: age,FHx, obesity, sedentary lifestyle •
Type 2 DM p
/
w DKA
(“ketosis-prone type 2 diabetes” or “Flatbush diabetes”): most often seen in nonwhite, ± anti-GAD Ab, eventually may not require insulin (
Endo Rev
2008;29:292) •
M
ature-
O
nset
D
iabetes of the
Y
oung (
MODY
): autosomal dom. forms of DM due to defects in insulin secretion genes; genetically and clinically heterogeneous (
NEJM
2001;345:971) •
Secondary causes of diabetes
: exogenous glucocorticoids, glucagonoma (3 Ds = DM, DVT, diarrhea), pancreatic (pancreatitis, hemochromatosis, CF, resection), endocrinopathies (Cushing’s disease, acromegaly), gestational, drugs (protease inhibitors, atypical antipsychotics)
Clinical manifestations
• Polyuria, polydipsia, polyphagia with unexplained weight loss; can also be asymptomatic
Complications
•
Retinopathy
nonproliferative
: “dot & blot” and retinal hemorrhages, cotton-wool/protein exudates
proliferative:
neovascularization, vitreous hemorrhage, retinal detachment, blindness
treatment: photocoagulation, surgery, intravitreal bevacizumab injections
•
Nephropathy
: microalbuminuria → proteinuria ± nephrotic syndrome → renal failure
diffuse glomerular basement membrane thickening/nodular pattern (Kimmelstiel-Wilson)
usually accompanied by retinopathy; lack of retinopathy suggests another cause
treatment: strict BP control using ACE inhibitors (
NEJM
1993;329:1456 & 351:1941;
Lancet
1997;349:1787) or ARBs (
NEJM
2001;345:851 & 861), low-protein diet, dialysis or transplant
•
Neuropathy
:
peripheral
: symmetric distal sensory loss, paresthesias, ± motor loss
autonomic:
gastroparesis, constipation, neurogenic bladder, erectile dysfxn, orthostasis
mononeuropathy
: sudden-onset peripheral or CN deficit (footdrop, CN III > VI > IV)
•
Accelerated atherosclerosis
: coronary, cerebral and peripheral arterial beds •
Infections
: UTI, osteomyelitis of foot, candidiasis, mucormycosis, necrotizing external otitis •
Dermatologic
: necrobiosis lipoidica diabeticorum, lipodystrophy, acanthosis nigricans
Outpatient screening and treatment goals
(
Diabetes Care
2012;35:1364)
• ✓ Hb
A1C
q3–6mo, goal <7% for most Pts. Can use goal Hb
A1C
≥7.5–8% if h/o severe hypoglycemia or other comorbidities. Microvascular & macrovascular complications ↓ by strict glycemic control in T1D (
NEJM
1993;329:997 & 2005;353:2643) & T2D (
Lancet
2009;373:1765;
Annals
2009;151:394).
• Microalbuminuria screening yearly with spot microalbumin/Cr ratio, goal <30 mg/g •
BP≤130/80
(? ≤140/85,
Archives
2012;172:1296), benefit of ACE-I;
LDL < 100
, TG <150, HDL >40; benefit of statins even w/o overt CAD (
Lancet
2003;361:2005 & 2004;364:685);
ASA
if age >50 () or 60 (
) or other cardiac risk factors (
Circ
2010;121:2694) • Dilated retinal exam yearly; comprehensive foot exam qy
Management of hyperglycemia in inpatients
(for ICU Pts: see “Sepsis”)
• Identify reversible causes/exacerbaters (dextrose IVF, glucocorticoids, postop, ↑ carb diet) • Dx studies: BG fingersticks (fasting, qAC, qHS; or q6h if NPO), Hb
A1C
• Treatment goals: avoid hypoglycemia, extreme hyperglycemia (>180 mg/dL) • Modification of outPt treatment regimen: In T1D, do not stop basal insulin (can → DKA).
In T2D: stopping oral DM meds generally preferred to avoid hypoglycemia or med interaction (except if short stay, excellent outPt cntl, no plan for IV contrast, nl diet)
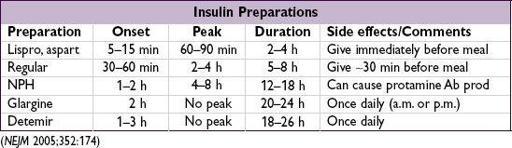
• InPt insulin: can use outPt regimen as guide; if insulin naïve:
total daily insulin = wt (kg) ÷ 2, to start; adjust as needed
give
1
/
2
of total daily insulin as basal insulin in long-acting form to target fasting glc
give other
1
/
2
as short-acting boluses (standing premeal & sliding scale corrective insulin)