Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (99 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.52Mb size Format: txt, pdf, ePub
• Adrenal CT or MRI; consider MIBG scintigraphy if CT/MRI, PET can be used to
localize nonadrenal mass, but usually easy to find
• Consider genetic testing in appropriate circumstances (bilateral, young Pt,FHx, extra-adrenal)
Treatment
• ɑ-blockade first (usually phenoxybenzamine) ± β-blockade (often propranolol) → surgery
• Preoperative volume expansion is critical due to possible hypotension after tumor excision
ADRENAL INCIDENTALOMAS
Epidemiology
• 4% of Pts undergoing abdominal CT scan have incidentally discovered adrenal mass; prevalence ↑ with age
Differential diagnosis
•
Nonfunctioning mass
: adenoma, cysts, abscesses, granuloma, hemorrhage, lipoma,
myelolipoma, primary or metastatic malignancy
•
Functioning mass
: pheochromocytoma, adenoma (cortisol, aldosterone, sex hormones), nonclassical CAH, other endocrine tumor, carcinoma •
Nonadrenal mass
: renal, pancreatic, gastric, artifact
Workup
(
NEJM
2007;356:601;
JCEM
2010;95:4106)
•
Rule out subclinical Cushing’s syndrome
in all Pts
using 1 mg overnight DST (Sp 91%). Abnormal results require confirmatory testing.
•
Rule out hyperaldosteronism
if hypertensive
w/ plasma aldo & renin (see above) •
Rule out pheochromocytoma
in ALL Pts
(b/c of morbidity unRx’d pheo) using 24-h urine fractionated metanephrines and catecholamines or plasma free metanephrines • Rule out metastatic cancer and infection by history or CT-guided biopsy if suspicious (in Pts w/ h/o cancer, ~50% of adrenal incidentalomas are malignant) • CT and MRI characteristics may suggest adenoma vs. carcinoma
Benign features:
size <4 cm; smooth margins, homogenous and hypodense appearance; unenhanced CT <10 Hounsfield units or CT contrast-medium washout >50% at 10 min. Can follow such incidentalomas w/ periodic scans.
Suspicious features:
size >4 cm or ↑ size on repeat scan; irregular margins, heterogeneous, dense or vascular appearance; h/o malignancy or young age (incidentaloma less common). Such incidentalomas warrant resection or repeat scan at short interval.
CALCIUM DISORDERS
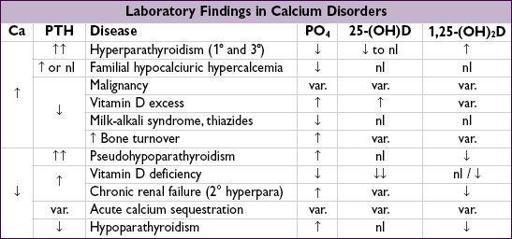
Pitfalls in measuring calcium
• Physiologically active Ca is free or ionized (ICa). Serum Ca reflects total calcium (bound + unbound) and ∴ influenced by albumin (main Ca-binding protein).
• Corrected Ca (mg/dL) = measured Ca (mg/dL) + {0.8 × [4 − albumin (g/dL)]}
• Alkalosis will cause more Ca to be bound to albumin (∴ total Ca may be normal but ↓ ICa) • Best to measure
ionized Ca directly
(but accuracy is lab dependent)
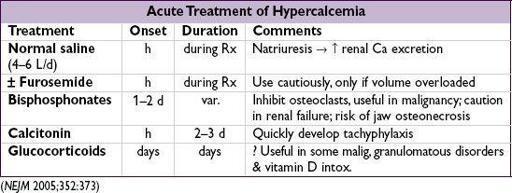
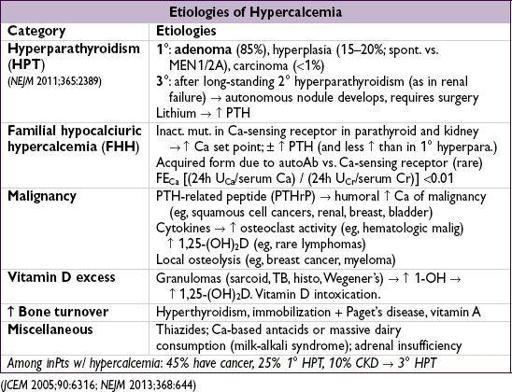
HYPERCALCEMIA
Clinical manifestations
(“bones, stones, abdominal groans and psychic moans”)
•
Hypercalcemic crisis
(usually when Ca >13–15): polyuria, dehydration, ΔMS
Ca toxic to renal tubules → blocks ADH activity, causes vasoconstriction and ↓ GFR → polyuria but Ca reabsorption → ↑ serum Ca → ↑ nephrotoxicity and CNS sx
• Osteopenia, fractures and osteitis fibrosa cystica (latter seen in severe hyperpara. only →
↑ osteoclast activity → cysts, fibrous nodules, salt & pepper appearance on X-ray)
• Nephrolithiasis, nephrocalcinosis, nephrogenic DI
• Abdominal pain, anorexia, nausea, vomiting, constipation, pancreatitis, PUD
• Fatigue, weakness, depression, confusion, coma, ↓ DTRs, short QT interval • 1° HPT: 80% asx, 20% nephrolithiasis, osteoporosis,
etc.
•
Calciphylaxis
(calcific uremic arteriopathy): calcification of media of small-to med-sized blood vessels of dermis & SC fat → ischemia and skin necrosis (
NEJM
2007;356:1049).
Associated w/ uremia, ↑ PTH, ↑ Ca, ↑ PO
4
and ↑ (Ca × PO
4
) product. Dx by biopsy.
Rx: aggressive wound care, keep Ca & PO
4
nl (goal <55), avoid vitamin Δ & Ca suppl. IV Na thiosulfate, cinacalcet, & parathyroidectomy controversial.
Overall portends a poor prognosis
Diagnostic studies
• Hyperparathyroidism and malignancy account for 90% of cases of hypercalcemia
hyperparathyroidism more likely if asx or chronic hypercalcemia
malignancy more likely if acute or sx; malignancy usually overt or becomes so in mos
• Ca, alb, ICa, PTH (may be inappropriately normal in 1° HPT & FHH), PO
4
;
↑ or high nl PTH: 24-h U
Ca
>200 mg → HPT; 24-h U
Ca
<100 mg & FE
Ca
<0.01 → FHH
↓ PTH: ✓ PTHrP, AΦ, & search for malig (eg, CT, mammogram, SPEP/UPEP) and ✓ vit D: ↑ 25-(OH)D → meds; ↑ 1,25-(OH)
2
D → granuloma (✓ CXR, ACE, r/o lymph)
Treatment of asymptomatic 1° HPT
(JCEM 2009;94:335)
• Surgery if: age <50 y; serum Ca >1 mg/dL >ULN; CrCl <60 mL/min, DEXA T score <-2.5
• If surgery declined/deferred, can Rx with bisphosphonates (↑ BMD but do not ↓ Ca & PTH) or cinacalcet (↓ Ca & PTH but may not ↑ BMD) • If not yet candidate for surgery: ✓ serum Ca & Cr annually and BMD q1–2y
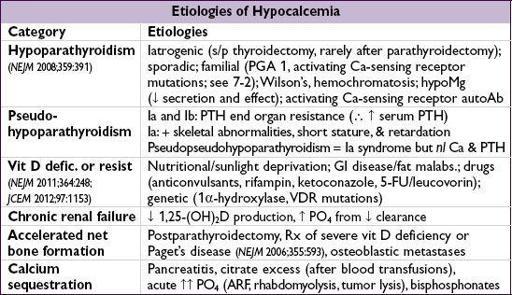
HYPOCALCEMIA
Clinical manifestations
•
Neuromuscular irritability
: perioral paresthesias, cramps,Chvostek’s
(tapping facial nerve → contraction of facial muscles),Trousseau’s
(inflation of BP cuff → carpal spasm), laryngospasm; irritability, depression, psychosis, ↑ ICP, seizures, ↑ QT
Other books
I'm With the Bears by Mark Martin
A Planet of Viruses by Carl Zimmer
Dark Light (The Dark Light Series) by S.L. Jennings
By a Thread by Jennifer Estep
On Folly Beach by Karen White
Whip Hands by C. P. Hazel
Amethyst by Heather Bowhay
Death of a Pumpkin Carver by Lee Hollis
My Only by Duane, Sophia
Rise Again by Ben Tripp