Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (41 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

• Painless hematochezia/BRBPR; can have abdominal cramping
• Usually stops spontaneously (~75%) but resolution may occur over hrs–days; ~20% recur
Diagnostic studies
• Colonoscopy: rapid prep w/ PEG-based solution via NGT (4–6 L over 2–4 h) • Arteriography ± tagged RBC scan if severe bleeding
Treatment
• Colonoscopy: epinephrine injection ± electrocautery (
NEJM
2000;342:78), hemoclip, banding • Arteriography: intra-arterial vasopressin infusion or embolization
• Surgery: if above modalities fail & bleeding is persistent & hemodynamically significant
INFLAMMATORY BOWEL DISEASE
Definition
•
Ulcerative colitis (UC)
: idiopathic inflammation of the colonic
mucosa
•
Crohn’s disease (CD)
: idiopathic
transmural
inflammation of the GI tract,
skip areas
• Indeterminate colitis: in 5–10% of chronic colitis, cannot distinguish UC vs. CD even w/ bx
Epidemiology & pathophysiology
(
NEJM
2009;361:2066;
Gastro
2011;140:1785)
• 1.4 million people in U.S.; prev 1:1000 UC & 1:3000 CD; ↑ incidence in Caucasians, Jews • Age of onset 15–30 y in UC and CD; CD is bimodal and has second peak at 50–70 y • Smokers at ↑ risk for CD, whereas nonsmokers & former smokers at ↑ risk for UC
• Genetic predisposition + disruption of intestinal barrier (epithelial or ↓ defenses) ± Δ in gut microbiota → acute inflam w/o immune downregulation or tolerance → chronic inflam
ULCERATIVE COLITIS (
NEJM
2011;365:1713;
Lancet
2012;380:1606)
Clinical manifestations
•
Grossly bloody diarrhea
, lower abdominal cramps, urgency, tenesmus •
Severe colitis
(15%): progresses rapidly over 1–2 wk with ↓ Hct, ↑ ESR, fever, hypotension, >6 bloody BMs per day, distended abdomen with absent bowel sounds • Extracolonic (>25%): erythema nodosum, pyoderma gangrenosum, aphthous ulcers, uveitis, episcleritis, thromboembolic events (esp. during a flare;
Lancet
2010;375:657), AIHA, seroneg arthritis, chronic hepatitis, cirrhosis, PSC (↑ risk cholangio CA, CRC)
Diagnosis
•
Colonoscopy
: involves rectum (95%) & extends proximally and
contiguously within colon
• Classify by location: proctitis (25–55%), left-sided colitis (50–70%) and pancolitis (20%) • Appearance: granular, friable mucosa with diffuse ulceration;
pseudopolyps
• Microscopy: superficial chronic inflammation; crypt abscesses & architectural distortion
Complications
•
Toxic megacolon
(5%): colon dilatation (≥6 cm on KUB), colonic atony, systemic toxicity, & ↑ risk of perf. Rx w/ IV steroids & broad-spectrum abx; surgery if fail to improve w/in 48–72 h • Stricture (5%): occurs in rectosigmoid after repeated episodes of inflammation
Prognosis
• 50% of Pts in remission at any given time; intermittent exacerbations in 90%; continual active disease in ~18%. Rate of colectomy at 10 y is 24%.
• Mortality rate of severe UC flare is <2%, & overall life expectancy in UC = non-UC Pts
CROHN’S DISEASE (
Lancet
2012;380:1590)
Clinical manifestations
•
Abdominal pain
, fever, malaise, wt loss •
Mucus-containing, nongrossly bloody diarrhea;
N/V, bloating, obstipation • ↓ albumin, ↑ ESR/CRP, ↓ Hct (due to Fe, B
12
, folate deficiency; chronic inflammation) • Extracolonic as in UC
Diagnosis
•
EGD/colonoscopy + small bowel imaging
(eg, video capsule endoscopy [if no stricture] or CT/MR-enterography); CD can affect
any
portion of GI tract with
skip lesions
• Classify by location: small bowel (47%), ileocolonic (21%), colonic (28%); upper tract rare •
Appearance: nonfriable mucosa, cobblestoning, aphthous ulcers, deep & long fissures
•
Microscopy: transmural inflammation
with mononuclear cell infiltrate, noncaseating granulomas (seen in <25% of mucosal biopsies), fibrosis, ulcers, fissures
Complications
•
Perianal disease
: fissures, fistulas, perirectal abscesses (up to 30% of Pts) •
Stricture
: small bowel, postprandial abd pain; can lead to complete SBO
•
Fistulas
: perianal, enteroenteric, rectovaginal, enterovesicular, enterocutaneous •
Abscess
: fever, tender abd mass, ↑ WBC;
steroids mask sx
, ∴ need high-level suspicion •
Malabsorption
: ileal disease/resection: ↓ bile acids abs → gallstones; ↓ fatty acid abs → Ca oxalate kidney stones; ↓ fat soluble vitamin abs → vit Δ deficiency → osteopenia
Prognosis
• Variable at 1 y:
50% in remission,
20% flared,
20% low activity,
10% chronic active • At 20 y, majority will have required some surgery; overall life expectancy is slightly ↓
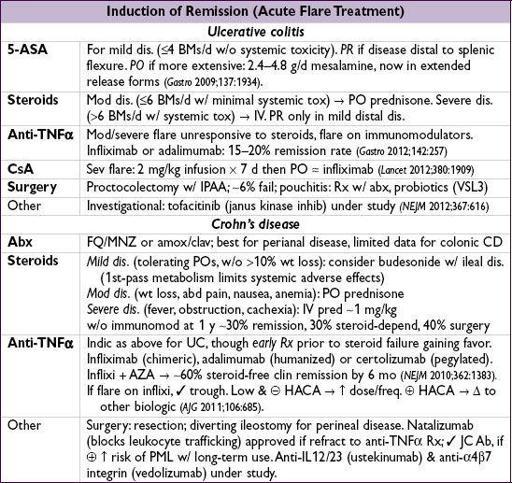
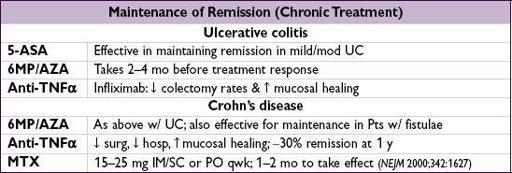
MANAGEMENT (
Gastro
2011;140:1827)
Initial evaluation
•
H&P
(✓ for intestinal & extraintestinal manifestations) and endoscopy as above •
Laboratory
: ESR, CRP, CBC, LFTs, Fe, B
12
, folate, vit D. Fecal calprotectin appears useful for Ddx IBD vs. IBS & may predict IBD flare (
Infl Bowel Dis
2012;18:2218).
•
Exclude other etiologies
: infectious/ischemic colitis, med adverse effect, intestinal lymphoma/carcinoma, colon cancer, IBS, vasculitis, Behçet’s, celiac disease, SIBO
•
Rule out infection
before treating with immunosuppressants and biologics
Goals of treatment
• Avoid NSAIDs (both UC and CD) • Induce remission of acute flare → maintain remission; mucosal healing 1° goal • Convention has been step up Rx (least → most toxic). Recent shift to early and/or combined immunomodulation to improve disease outcome (
Lancet
2008;371:660;
NEJM
2010;362:1383).
Complications of therapy
(
Clin Gastro Hep
2009;7:874)
•
Anti-TNF
α: reactivation TB; must doc PPD prior to Rx. Exclude viral hepatitis. Small ↑’d risk of NHL. Other: infusion rxn; lupus-like rxn, psoriasis, MS, CHF.
PPD prior to Rx. Exclude viral hepatitis. Small ↑’d risk of NHL. Other: infusion rxn; lupus-like rxn, psoriasis, MS, CHF.
•
6MP/AZA
: BM suppression, lymphoma, pancreatitis, hepatitis; ✓ TPMT genotype prior to dosing to ↓ risk of generation of toxic metabolites •
5-ASA
: diarrhea, abd pain, pancreatitis. If sx, consider 3-d holiday.
Cancer screening
(
Gastro
2010;138:738)
•
Colon cancer
: risk in UC
2% at 10 y,
8% at 20 y, ~18% at 30 y. Similar for colonic CD, plus risk of small bowel cancer as well. Dysplasia best marker for risk. Other risk factors include: PSC, FHx, greater extent of disease, stricture, & pseudopolyps.
FHx, greater extent of disease, stricture, & pseudopolyps.
•
Surveillance
:
colonoscopy
w/ random bx 8 y after dx to eval for dysplasia, q1–3y thereafter based on risk factors. If high-grade dysplasia or dysplasia assoc. lesion/mass → colectomy. Chemoprophylaxis: 5-ASA & ursodeoxycholic acid (if PSC) ? beneficial (
AJG
2011;106:731;
Aliment Pharmacol Ther
2012;35:451).
INTESTINAL ISCHEMIA
ACUTE MESENTERIC ISCHEMIA (25%)
Etiologies
•
SMA embolism
(50%): from LA (AF), LV (↓ EF) or valves; SMA most prone to embolism •
Nonocclusive mesenteric ischemia
(25%): transient intestinal hypoperfusion due to ↓ CO, atherosclerosis, sepsis, drugs that ↓ gut perfusion (pressors, cocaine, dig, diuretics) •
SMA thrombosis
(10%): usually at site of atherosclerosis, often at origin of artery •
Venous thrombosis
(10%): hypercoagulable states, portal hypertension, IBD, malignancy, inflammation (pancreatitis, peritonitis), pregnancy, trauma, surgery •
Focal segmental ischemia of the small bowel
(<5%): vascular occlusion to small segments of the small bowel (vasculitis, atheromatous emboli, strangulated hernias, XRT)
Clinical manifestations
•
Occlusive: sudden abd pain out of proportion to abdominal tenderness on exam
at least
initially
(2–4 h) until severe ischemia → frank infarction w/ peritoneal signs • Nonocclusive: abd distention & pain, though up to 25% may be pain-free,N/V; often in setting of CHF ± h/o chronic mesenteric ischemia sx • Hematochezia due to mucosal sloughing (right colon supplied by SMA)