Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (43 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
4.66Mb size Format: txt, pdf, ePub
↑ lipase
: more specific than amylase
false: renal failure, other abd process, diabetic ketoacidosis, HIV, macrolipasemia
ALT >3 × ULN suggests gallstone pancreatitis (
Am J Gastro
1994;89:1863); AΦ, bili not helpful
Other labs (see “Prognosis”): ↑ WBC, ↑ or ↓ Hct, ↑ BUN, ↓ Ca, ↑ glc, ↑ CRP
• Imaging studies
KUB/CXR: can see “sentinel loop” air in small bowel in LUQ, atelectasis, effusion
Abd CT
: not required for dx, but test of choice to make dx. Helps exclude other dx, stage severity, & r/o complications. CT w/ IV contrast on day 3 of presentation in severe cases to evaluate for pancreatic necrosis (avoid on presentation b/c theoretical concern of ↑ necrosis w/ IV contrast; defer if concomitant AKI).
Abd U/S
: typically not useful to visualize pancreas (obscured by bowel gas), but helpful to investigate biliary etiology (ie, gallstones and BD dilatation); can see pseudocyst
MRI/MRCP: can detect necrosis; also used to assess for stones & ductal disruption
Endoscopic U/S (EUS): limited role acutely; useful for occult biliary disease (microlithiasis)
Treatment
(
Lancet
2008;371:143;
AJG
2012;107:1146)
• Supportive therapy: in mild cases, bowel rest is usually sufficient
Fluid resuscitation
LR may be superior to NS (↓ SIRS, CRP at 24 h; contraindicated if ↑ Ca); at least 250 mL/h, may need up to
10 L
/
d
if severe; titrate to UOP ≥0.5 mL/kg/h
Nutrition
: if mild, initiate oral nutrition when pain, nausea allow.
If severe and NPO >7 d expected, early (w/in 48 h) enteral nutrition indicated and preferred over TPN; ↓ infectious complications & disease severity, & trend toward ↓ mortality (
BMJ
2004;328:1407). Ideally NJ tube, but NG okay.
Analgesia
: IV meperidine, morphine, hydromorphone (theoretical risk of sphincter of Oddi spasm by opiates, but has not been shown to adversely affect outcome)
• Prophylactic systemic
abx
(eg, imipenem) to ↓ mortality & prevent conversion of sterile to infected necrosis controversial (
Am J Surg
2009;197:806;
Gastro
2007;132:2022); ? reserve for severe pancreatitis w/ >30% necrosis by CT, & no >14 d • Debridement: infected necrosis usually requires percut, endoscopic or surgical debridement. Improved outcomes by delaying surgery ≥2 wk if possible to allow organization of necrosis. CCY if gallstones (w/in 48 h if mild, o/w w/in 14 d;
Surg
2009;145:260;
Ann Surg
2010;251:615) • ERCP + sphincterotomy: in acute setting, reserved for severe cholangitis/sepsis and T bili >5 (ie, presumptive obstructive BD stone). Otherwise, early ERCP does not reduce risk of local or systemic pancreatitis complications (
Ann Surg
2007;245:10).
Complications
• Systemic: shock, ARDS, renal failure, GI hemorrhage, DIC
• Metabolic: hypocalcemia, hyperglycemia, hypertriglyceridemia •
Acute fluid collection
(30–50%): seen early, no capsule, no Rx required •
Pseudocyst
(10–20%): fluid collection, persists for 4–6 wk, encapsulated suggested by persistent pain & elevation of amylase or lipase, or mass on exam most resolve spont.; if >6 cm or persists >6 wk + pain → endo/perc/surg drainage •
Sterile pancreatic necrosis
(20%): area of nonviable pancreatic tissue ? prophylactic abx (see above); supportive measures, surgery if Pt unstable •
Infection
(5% of all cases, 30% of severe): usually 2° enteric GNR
infected pancreatic necrosis
: new SIRS after 7 d typical; perc drainage followed by min invasive surg debridement or endoscopic necrosectomy superior to open necrosectomy; FNA no longer routinely recommended (
Pancreas
2012;41:1176)
pancreatic abscess
: circumscribed collection of pus (usually w/o pancreatic tissue) treat with abx + drainage (CT-guided if possible), usually seen ≥4 wk into course
•
Ascites or pleural effusion
: occurs due to disrupted pancreatic duct; consider early ERCP w/ stent across duct; can also occur from draining pseudocyst
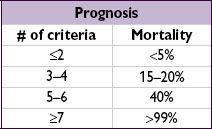
Prognosis
(
Gastro
2007;132:2022)
• Severe pancreatitis (20%) = organ failure
or
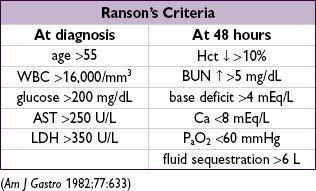
local complications (necrosis, pseudocyst) • Scoring systems: HAPS, BISAP, APACHE II, Ranson’s criteria, CT Severity Index
HAPS
: no abd tenderness or rebound on exam plus nl Hct and Cr on admission predicts non-severe course w/ 98% accuracy (
Clin Gas Hep
2009;6:702)
BISAP
: 5-point scoring system on admission (BUN >25, GCS <15, SIRS, age >60, and pleural effusion) identifies Pts at risk for ↑’d mortality (
Am J Gastro
2009;104:966)
APACHE II
(
www.mdcalc.com/apache-ii-score-for-icu-mortality
): severe if score ≥8
Chronic pancreatitis
(
Lancet
2011;377:1184)
• 70–80% due to EtOH, also consider autoimmune pancreatitis. Smoking major risk factor.
• Often, but not always, recurrent acute attacks → inflammatory infiltrate → fibrosis → exocrine then endocrine insufficiency (eg, diabetes) • Sxs include epigastric pain, N/V; over time will be painless and p/w steatorrhea and wt loss • Amylase/lipase ↑ early, but may be nl later.fecal fat, ↓’d stool elastase & chymotrypsin, Ca
2
+
in pancreas on KUB/CT.
• ERCP/MRCP/EUS high Se for dx: stricture, dilated ducts, honeycombing of parenchyma • Treatment is low-fat diet and enzyme replacement. Avoid EtOH & tobacco. Analgesia w/ NSAID ± mild opioid (eg, tramadol). Surgery in selected cases.
ABNORMAL LIVER TESTS
Tests of hepatocellular injury or cholestasis
•
Aminotransferases
(AST, ALT): intracellular enzymes released 2° necrosis/inflammation
ALT more specific for liver than is AST (heart, skeletal muscle, kidney, brain, RBC/WBC)
ALT > AST → viral hepatitis or fatty liver/nonalcoholic steatohepatitis (precirrhotic)
AST: ALT >2:1 → alcoholic hepatitis, cirrhosis; nonhepatic source
ALT/AST >15× ULN → etiologies of acute liver failure (↑↑↑ LDH → ischemia/toxic)
•
Alkaline phosphatase
(AΦ): enzyme bound in hepatic canicular membrane
besides liver, also found in bone, intestines, kidney and placenta
confirm liver origin with: ↑ 5′-NT, ↑ GGT or AΦ heat fractionation
↑ levels seen with biliary obstruction or intrahepatic cholestasis (eg, hepatic infiltration)
Tests of hepatic function
•
Albumin
: marker for liver protein synthesis, ↓ slowly in liver failure (t
1
/2
~20 d) •
Prothrombin time
(PT): depends on synthesis of coag factors by liver (except FVIII); b/c t
1
/2
of some factors (eg, V, VII) is short, ↑ PT can occur w/in hrs of liver dysfxn •
Bilirubin
: product of heme metab (unconjugated, “indirect”) carried by alb to liver where taken up for conjugation (“direct”) to make soluble, then excreted into bile; most sensitive test to detect parenchymal disease; in those w/ normal LFTs, high nl Tbili (? marker of ↑ heme oxygenase) a/w ↓ resp disease & death (
JAMA
2011;305:691)
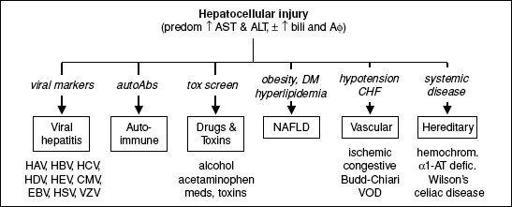
Patterns of liver injury
•
Hepatocellular
: ↑↑ aminotransferases, ± ↑ bilirubin or AΦ
↑↑↑ ALT & AST (>1000): severe viral hepatitis, drugs, ischemia, Wilson’s, AIH
•
Cholestasis
: ↑↑ AΦ and bilirubin, ± ↑ aminotransferases •
Isolated hyperbilirubinemia
: ↑↑ bilirubin (direct or indirect), nl AΦ and aminotransferases •
Infiltrative
: ↑ AΦ, ± ↑ bilirubin or aminotransferases •
Jaundice
is a clinical sign seen when bilirubin >2.5 mg/dL (esp. in sclera or under
tongue); if hyperbilirubinemia conjugated → ↑ urine bilirubin
Figure 3-3
Approach to abnormal liver tests with hepatocellular pattern
Other books
Stirring It Up with Molly Ivins by Ellen Sweets
Fletcher Pratt by Alien Planet
The Quivering Tree by S. T. Haymon
Dark Moon Walking by R. J. McMillen
The Mysterious Mr Quin by Agatha Christie
Black Wolf (2010) by Brown, Dale
Hit & Miss by Derek Jeter
My Accidental Jihad by Krista Bremer
The Billionaire's Marriage Bargain by Carole Mortimer
Lost and Found by Jennifer Bryan Yarbrough