Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (36 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
4.02Mb size Format: txt, pdf, ePub
Fluids & vasoactive drugs
•
Early goal-directed therapy
(“Rivers Protocol,”
NEJM
2001;345:1368), confirm. trials pending
Insert arterial & central venous lines (
NEJM
2007;356:e21; PAC not needed) and ✓ MAP, CVP & S
cv
O
2
(central venous O
2
sat, nl 60–80%) which measures O
2
consumption vs. delivery (less invasive than mixed venous) w/ low S
CV
O
2
→ ↓ O
2
delivery (↓ S
a
O
2
, nl S
a
O
2
but ↓ CO or anemia) or excessive O
2
consumption
Target MAP ≥65 mmHg, CVP 8–12 mmHg, & UOP ≥0.5 mL/kg/h using fluid (eg, 500 mL NS q30min) and vasopressors as needed
Target S
cv
O
2
≥70% using PRBCs & inotropes (dobutamine, ↑ dose as needed q15min)
When done w/in first 6 h for severe sepsis & septic shock, 42% ↓ mortality
• Lactate clearance (≥20% / 2 h) as effective as S
cv
O
2
to guide resuscitation (
JAMA
2010;303:739) • Crystalloid better than colloid for resuscitation (
NEJM
2004;350:2247 & 2012;367:124 & 1901) • Norepi ↓ arrhyth. & mort. c/w dopamine (
NEJM
2010;362:779;
Crit Care Med
2012;40:725) • Vasopressin added to low-dose norepinephrine not superior to high-dose norepinephrine (
NEJM
2008;358:877); consider if HoTN refractory to catecholamine vasopressors • Use PRBC w/ caution, may ↑ mortality/morbidity, ↑ risk of ARDS (
Crit Care Med
2005;33:1191); ∴ goal Hb 7 unless active cardiac ischemia (
NEJM
1999;340:409) • After early resuscitation, if ALI/ARDS, target CVP 4–6 mmHg as additional fluids may be harmful → ↑ ventilator/ICU days (
NEJM
2006;354:2564;
Chest
2008;133:252) • Pulse pressure variation >13% with respiration → likely volume-responsive (
Chest
2008;133:252); only validated in passive, intubated Pts and studied in higher tidal volumes
Antibiotics
• Start empiric IV abx w/in 1 h of recognition of severe sepsis or septic shock; every hour delay in abx admin a/w 8% ↑ in mortality (
Crit Care Med
2006;34:1589) • If possible, obtain 2 sets of BCx before urgently starting abx (but do not delay abx) • Typically want broad gram-positive and gram-negative coverage, including MRSA and highly resistant gram-negative bacilli ± anaerobes
Steroids
(
NEJM
2003;348:727;
JAMA
2009;301:2362)
• Cortisol secretion helps predict mortality, but treatment of adrenal insufficiency is unproven (
JAMA
2000;283:1038;
NEJM
2008;358:111) • Earlier study showed
possible
mortality benefit w/in 8 h of severe septic shock (SBP <90 for >1 h despite fluids & pressors) if post ACTH stim cortisol Δ ≤ 9 µg/dL (
JAMA
2002;288:862) • No mortality benefit to early (<72 h) empiric corticosteroids in all Pts w/ septic shock, regardless of ACTH stim; faster resolution of shock, more superinfection (
NEJM
2008;358:111) • ? hydrocortisone 50–100 q6–8h ± fludrocortisone 50 µg daily in septic shock refractory to fluids & pressors, regardless of ACTH stim (
Crit Care Med
2008;36:296)
Activated protein C
• No longer FDA approved, no improvement in mortality (
NEJM
2012;366:2055)
Intensive glycemic control
(
NEJM
2010;363:2540)
• No evidence of improved outcomes in MICU population w/ intensive glycemic control • Intensive glycemic control to goal 80–110 mg/dL in
surgical
ICU population → mortality benefit, greatest if >3-d ICU stay (
NEJM
2001;345:1359) • Repeat studies suggest intensive glycemic control → either no Δ or ↑ increased mortality, and definite ↑ hypoglyc. (
JAMA
2008;300:933;
NEJM
2006;354:449; 2008;358:125; 2009;360:1283) • Hypoglycemia associated with mortality (
NEJM
2012;367:1108) • Reasonable to keep glc <150 mg/dL in severe sepsis, using validated protocol (
Crit Care Med
2008;36:296)
NOTES
ESOPHAGEAL AND GASTRIC DISORDERS
DYSPHAGIA
Definitions
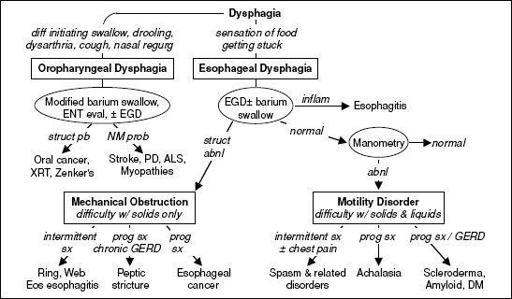
• Oropharyngeal: inability to propel food from mouth through UES into esophagus • Esophageal: difficulty swallowing & passing food from esophagus into stomach
Figure 3-1
Etiologies of and approach to dysphagia (
NCP Gastrohep
2008;5:393;
Neurogastro
2012;24:57)
Achalasia
• Etiologies: idiopathic (most common), pseudoachalasia (due to GE jxn tumor), Chagas • Sx: dysphagia (solid & liquid), chest pain (
1
/
3
of Pts), regurgitation • Dx: barium swallow → dilated esophagus w/ distal “bird’s beak” narrowing; manometry → simultaneous, low amplitude contractions of esophageal body, incomplete relaxation of lower esophageal sphincter (± LES hypertension); EGD → r/o pseudoachalasia (retroflex) • Rx: expert pneumatic dilation (≤4% eso perf)lap Heller myotomy (
NEJM
2011;364:1868)
Other esophageal disorders
• Webs (upper/mid esoph; congenital, GVHD, Fe-defic anemia); Rings (lower; ? due to GERD); Zenker’s diverticulum (pharyngoesoph jxn); dx w/ barium swallow; Rx: endo/surg • Infxn esophagitis: odynophagia > dysphagia; often immunosupp w/
Candida
, HSV, CMV
• Pill esophagitis: odynophagia > dysphagia; NSAID, KCl, bisphosp., doxy & tetracycline • Eosinophilic esophagitis (
Clin Gastro & Hep
2012;10:1066): seen in young or middle-aged, predom. Dx req >15 eos/hpf on bx & exclude GERD (eg, empiric PPI trial). Rx: 3
D
s:
D
iet (elim milk, soy, eggs, wheat, nuts, fish);
D
rugs (swallow inh steroids),
D
ilation
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
Pathophysiology
• Excessive transient relaxations of lower esophageal sphincter (LES) or incompetent LES
• Mucosal damage (esophagitis) due to prolonged contact w/ acid can evolve to stricture • Risk factors: hiatal hernia, obesity, gastric hypersecretory states, delayed emptying • Precipitants: supine position, fatty foods, caffeine, alcohol, cigarettes, CCB, pregnancy
Clinical manifestations
• Esophageal:
heartburn
, atypical chest pain, regurgitation, water brash, dysphagia • Extraesophageal:
cough
, asthma (often poorly controlled), laryngitis, dental erosions
Diagnosis
(
Gastro
2008;135:1383;
Am J Gastro
2010;105:747;
Annals
2012;157:808)
• Based on hx & empiric trial of PPI (Se & Sp: 78% & 54%) (
Annals
2004;140:518) • EGD if: (1) failure to respond to bid PPI; (2)
alarm features
: dysphagia, vomiting, wt loss, evid of blood loss; or ? (3)>50 y w/ sx ≥5 y + nocturnal sx, hiatal hernia, obesity, cigs • If dx uncertain & EGD nl → high res manometry w/ 24-h esoph pH monitoring ± impedance
Treatment
(
NEJM
2008;359:1700)
• Lifestyle: avoid precipitants, lose weight, avoid large & late meals, elevate head of bed • Medical: PPI achieve relief in 80–90% (titrate to lowest dose that achieves sx control)surgery among Pts who initially respond to acid suppression (
JAMA
2011;305:1969) • Refractory: confirm w/ pH testing: if acidic or sx correlate w/ reflux episodes → surgical fundoplication (implantation of magnetic esophageal sphincter device being studied;
NEJM
2013;368:719); if nl pH or no sx correlation → TCA, SSRI or baclofen (
Gastro
2010;139:7.e3)
Complications
(
NEJM
2009;361:2548;
Gastro
2011;140:1084 & e18)
• Barrett’s esophagus: dx by bx of intestinal metaplasia above GE jxn. Screen for BE if ≥2 of the following risk factors: >50 y, male, white, chronic GERD, hiatal hernia, high BMI.
Other books
Unbidden (The Evolution Series) by Hughey, Jill
Insomnia by Johansson, J. R.
Aramus by Eve Langlais
Infatuated by Elle Jordan
The Glitter Dome by Joseph Wambaugh
Prom and Prejudice by Stephanie Wardrop
Season of Shadows by Yvonne Whittal
Suddenly, a Knock on the Door: Stories by Etgar Keret, Nathan Englander, Miriam Shlesinger, Sondra Silverston
Thaw (Detective Ellie MacIntosh) by Watterson, Kate
The Cruiser by David Poyer