Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (38 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

Workup
•
History
:
where
(anatomic location) &
why
(etiology)
acute or chronic, prior GIB, # of episodes, other GI dx
hematemesis, vomiting
prior
to hematemesis (Mallory-Weiss), melena, hematochezia
abdominal pain, wt loss, anorexia, Δ in stool caliber
gastric irritants (ASA/NSAIDs), antiplatelet drugs, anticoagulants, known coagulopathy
alcohol (gastropathy, varices), cirrhosis, known liver disease, risk factors for liver disease
abdominal/rectal radiation, history of cancer, prior GI or aortic surgery
•
Physical exam
:
VS most important, orthostatic
D
s, JVP
localizable abd tenderness, peritoneal signs, masses, LAN, signs of prior surgery
signs of liver disease (hepatosplenomegaly, ascites, etc.)
rectal exam: masses, hemorrhoids, anal fissures, stool appearance, color, occult blood
pallor, jaundice, telangiectasias (alcoholic liver disease or hered. hemor. telangiectasia)
•
Lab studies
: Hct (
may be normal
in first 24 h of acute GIB before equilibration)
↓ 2–3% → 500 mL blood loss; low MCV → Fe deficient and chronic blood loss; plt,
PT
,
PTT
; BUN/Cr (ratio >36 in UGIB b/c GI resorption of blood ± prerenal azotemia); LFTs
Diagnostic studies
•
Nasogastric tube
can aid localization:
fresh blood
→ active UGIB;
coffee grounds
→ recent UGIB;
nonbloody bile
→ ? lower source, but does not exclude active UGIB (~15% missed);occult blood testing of no value •
UGIB: EGD
w/in 24 h for dx and poss Rx; ↓ LOS & need for surgery, consider erythro 250 mg IV 30 min prior → empty stomach of blood → ↑ Dx/Rx yield (
Am J Gastro
2006;101:1211) • LGIB:
first
r/o UGIB before attempting to localize presumed LGIB (10–15% actually UGIB, 3–5% small bowel),
then
colonoscopy (identifies cause in >70%); consider rapid purge w/ PEG solution 4 L over 2 h; no clear benefit of colonoscopy w/in 12 vs. 36–60 h (
AJG
2010;105;2636); CT angio promising (
Radiology
2010;262:109) • Unstable or recurrent UGIB & LGIB:
tagged RBC scan
: can localize bleeding rates ≥0.1 mL/min for surg but unreliable
arteriography
: can localize if bleeding rates ≥0.5 mL/min and can Rx (coil, vaso, glue) emergent exploratory laparotomy (last resort)
Obscure GIB
(
Gastro
2007;133:1694;
GIE
2010;72:471)
•
Definition
: continued bleeding (melena, hematochezia) despite EGD & colo; 5% of GIB
EGD & colo; 5% of GIB
•
Etiologies
: Dieulafoy’s lesion, small bowel angiodysplasia, ulcer or cancer, Crohn’s disease, aortoenteric fistula, Meckel’s diverticulum (2% of pop., remnant of vitelline duct w/ ectopic gastric mucosa), hemobilia •
Diagnosis
: repeat EGD w/ push enteroscopy/colonoscopy when bleeding is active
If, video capsule to evaluate small intestine (
Gastro
2009;137:1197)
If still, consider
99m
Tc-pertechnetate scan (“Meckel’s scan”), enteroscopy (single-balloon, double-balloon or spiral), tagged RBC scan and arteriography
DIARRHEA, CONSTIPATION AND ILEUS
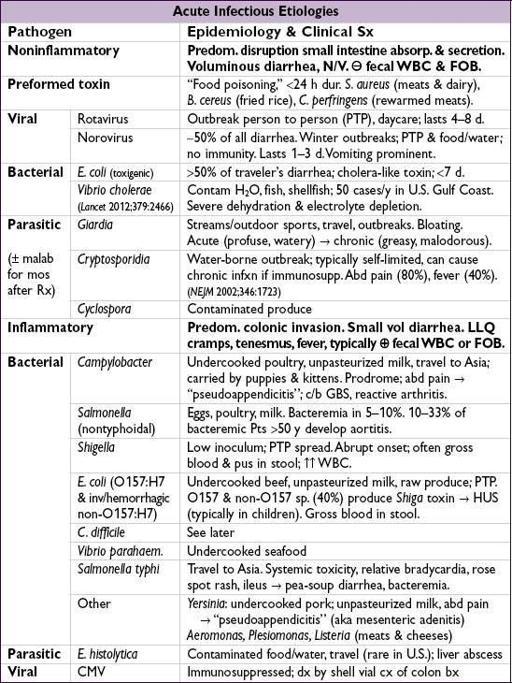
ACUTE DIARRHEA (<4 wk)
Evaluation
(
NEJM
2009;361:1560;
Gastro
2009;136:1874)
•
Hx
: stool freq, bloody, abd pain, duration of sxs [~1 wk for viral & bacterial (except
C. diff
), >1 wk for parasitic], travel, food, recent abx •
PEx
: vol depletion (VS, UOP, axillae, skin turgor, MS), fever, abd tenderness, ileus, rash •
Further evaluation if
warning signs
:
fever, signific abd pain, blood or pus in stools, >6 stools/d, severe dehydration, immunosupp, elderly, duration >7 d, hosp-acquired • Etiology established in only ~3% of community-acquired diarrhea •
Laboratory
: fecal WBC (high false &
& ; ✓ fecal calprotectin or lactoferrin Se/Sp >90%), stool cx, BCx, lytes,
; ✓ fecal calprotectin or lactoferrin Se/Sp >90%), stool cx, BCx, lytes,
C. diff
(if recent hosp or abx), stool O&P (if >10 d, travel to endemic area, exposure to unpurified H
2
O, community outbreak, daycare, HIV or MSM)
or MSM)