Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (33 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
11.22Mb size Format: txt, pdf, ePub
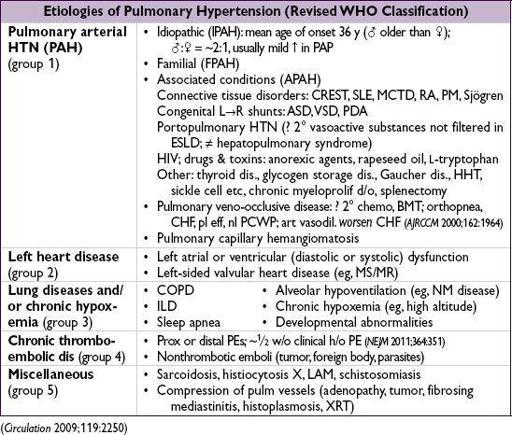
PULMONARY HYPERTENSION (PHT)
PA mean pressure >25 mmHg at rest
Pathobiology
(
NEJM
2004;35:1655)
• Smooth muscle & endothelial cell proliferation; mutations in bone morphogenic protein receptor 2 (
BMPR2
) in
50% familial &
26% sporadic cases of IPAH (
NEJM
2001;345:319) • Imbalance between vasoconstrictors and vasodilators
↑ vasoconstrictors: thromboxane A
2
(TXA
2
), serotonin (5-HT), endothelin-1 (ET-1)
↓ vasodilators: prostacyclin (PGI
2
), nitric oxide (NO), vasoactive peptide (VIP)
• In situ thrombosis: ↑ TXA
2
, 5-HT, PAI-1; ↓ PGI
2
, NO, VIP, tissue plasminogen activator
Clinical manifestations
• Dyspnea, exertional syncope (hypoxia, ↓ CO), exertional chest pain (RV ischemia) • Symptoms of R-sided CHF (eg, peripheral edema, RUQ fullness, abdominal distention) • WHO class: I=asx w/ ordinary activity; II=sx w/ ord. activ.; III=sx w/ min activ.; IV=sx at rest
Physical exam
• PHT: prominent P
2
, R-sided S
4
, RV heave, PA tap & flow murmur, PR (Graham Steell), TR
• ± RV failure: ↑ JVP, hepatomegaly, peripheral edema
Diagnostic studies & workup
(
Circ
2009;119:2250)
•
IPAH yearly incidence
1–2 per million
, ∴
r/o 2
°
causes
• CXR and high-resolution chest CT: dilatation & pruning of pulmonary arteries, enlargement of RA and RV; r/o parenchymal lung disease • ECG: RAD, RBBB, RAE (“P pulmonale”), RVH (Se 55%, Sp 70%) • PFTs: ↓ D
L
co, mild restrictive pattern; r/o obstructive and restrictive lung disease • ABG & polysomnography: ↓ P
a
O
2
and S
a
O
2
(esp. w/ exertion), ↓ P
a
CO
2
, ↑ A-a gradient; r/o hypoventilation and OSA • TTE: ↑ RVSP (but over or under by ≥10 mmHg in
1
/
2
of PHT Pts;
Chest
2011;139:988), flattened (“D”) septum, TR, PR; r/o LV dysfxn, MV disease and congenital heart disease • RHC: ↑ RA, RV, & PA pressures, nl PCWP (unless due to L-sided heart disease), ↑ transpulm gradient (PAP-PCWP >12–15, but can be nl if due to LV or valvular dis.), ↑ PVR, ↓ CO; r/o ↑ L-sided pressures shunt • CTA (large/med vessel), V/Q scan (small vessel to r/o CTEPH), ± pulmonary angiogram: r/o PE and chronic thromboembolic disease • Vasculitis labs: ANA (~40%in PAH), RF, anti-Scl-70, anticentromere, ESR
• LFTs & HIV: r/o portopulmonary and HIV-associated PAH
• 6-min walk test (6MWT) or cardiopulmonary exercise testing to establish fxnl capacity
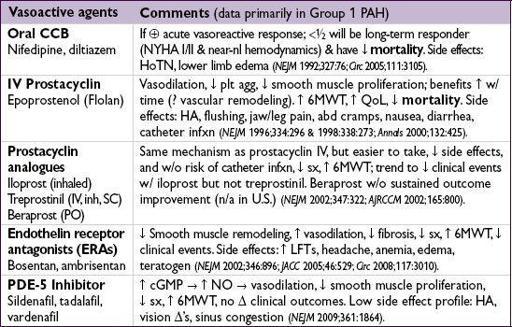
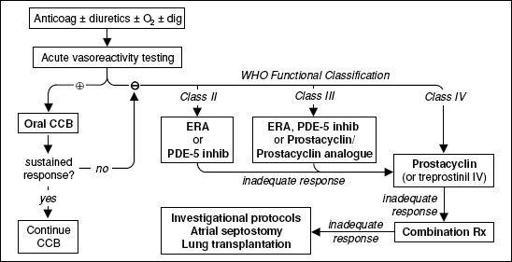
Treatment
(
NEJM
2004;351:1425;
JIM
2005;258:199;
Circ
2009;119:2250)
• Principles 1) prevent and reverse vasoactive substance imbalance and vascular remodeling 2) prevent RV failure: ↓ wall stress (↓ PVR, PAP, RV diam); ensure adeq. systemic DBP
•
Supportive
Oxygen: maintain S
a
O
2
>90–92% (reduces vasoconstriction)
Diuretics: ↓ RV wall stress and relieve RHF sx;
gentle
b/c RV is preload dependent
Digoxin: control AF, ? counteract neg. inotropic effects CCB
Dobutamine and inhaled NO for decompensated PHT
Anticoagulation: ↓ VTE risk of RHF; ? prevention of
in situ
microthrombi; ? mort. benefit even if in NSR (
Circ
1984;70:580;
Chest
2006;130:545)
•
Vasodilators
(right heart catheterization prior to initiation)
acute vasoreactivity test:
use inhaled NO, adenosine or prostacyclin to identify Pts likely to have a long-term response to oral CCB (vasoreactive response defined as ↓ PAP ≥10 mmHg to a level <40 mmHg with ↑ or stable CO); ~10% Pts are acute responders; no response → still candidates for other vasodilators (
NEJM
2004;351:1425)
• Treat underlying causes of 2° PHT; can use vasodilators, although little evidence • Refractory PHT:
balloon atrial septostomy: R→L shunt causes ↑ CO, ↓ S
a
O
2
, net ↑ tissue O
2
delivery
lung transplant (single or bilateral); heart-lung needed if Eisenmenger physiology
Figure 2-5 Treatment of PAH (modified from
JACC
2009;54:S78)
Management of ICU patient
• Avoid overly aggressive volume resuscitation • Caution with vasodilators if any L-sided dysfunction • May benefit from inotropes/chronotropes • Consider fibrinolysis if acute, refractory decompensation (eg, TPA 100 mg over 2 h)
Prognosis
• Median survival after dx ~2.8 y; PAH (all etiologies): 2-y 66%, 5-y 48% (
Chest
2004;126:78-S) • Poor prognostic factors: clinical evidence of RV failure, rapidly progressive sx, WHO (modified NYHA) class IV, 6MWT <300 m, peak VO
2
<10.4 mL/kg/min, ↑ RA or RV or RV dysfxn, RA >20 or CI <2.0, ↑ BNP (
Chest
2006;129:1313) • Lung transplant: 1-y survival 66–75%; 5-y survival 45–55% (
Chest
2004;126:63-S)
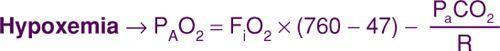
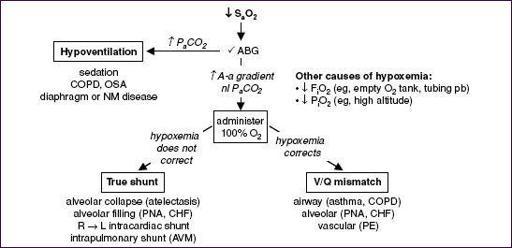
RESPIRATORY FAILURE
•
A-a gradient = P
A
O
2
– P
a
O
2
: normal (
on room air
) = “4 + age/4” or “2.5 + (0.2 × age)” hypoxemia + normal A-a gradient → problem is excess P
a
CO
2
(ie, hypoventilation)
•
V/Q mismatch
and
shunt
represent spectrum w/ both coexisting in alveolar disease
100% O
2
can overcome V/Q mismatch but not large shunt b/c sigmoidal Hg-O
2
curve
Figure 2-6 Workup of acute hypoxemia
Other books
Angel Dust by Sarah Mussi
Angel's Messiah by Melanie Tomlin
The Oneiro Rangers: First Night by Erwin Blackthorn
Nessa (Broken Sisters #1) by Brennan, M.
Safe and Sound by K. Sterling
Unexploded by Alison MacLeod
The Collected Joe Abercrombie by Abercrombie, Joe
Rock Me : Wicked by Arabella Quinn
Fighting to Stay (Fighting Madly Book 2) by Ziegler, S.L.
Bono by Michka Assayas, Michka Assayas