Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (115 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
8.53Mb size Format: txt, pdf, ePub
Etiologies
• Infections (types II & III): viral (
HCV
, HBV, HIV, HAV, EBV, CMV), bacterial (endocarditis, strep, etc.), fungal (coccidiomycosis, etc.) and parasitic (malaria, amoebiasis) • Hematologic diseases
type I: MM, CLL, Waldenström’s
type II: B-cell lymphomas, solid organ malignancies
• Autoimmune syndromes (type III > II):
Sjögren’s syndrome
, SLE, RA, PAN
• Essential (idiopathic) in 10% of cases
• Renal transplant recipients (Clin Nephrol 2008;69:239)
Pathophysiology
• Chronic immune stimulation and/or lymphoproliferation → cryoglobulin generation • Type I: cryo precipitation in microcirculation →
hyperviscosity
&
vascular occlusion
• Types II/III: defective/insufficient immune complex (IC) clearance → IC-mediated inflammation of blood vessels w/ complement activation →
vasculitis
Clinical manifestations
(systemic sx usually due to type II
> III)
• Most patients with cryoglobulinemia are asx
• Type I: hyperviscosity (cold worsens sx) → H/A, visual disturbance, livedo, digital ischemia • Type II: vasculitis (sx not affected by cold exposure)
General:
weakness
, low-grade fever
Dermatologic (54–80%): lower extremity
purpura
, livedo reticularis, leg ulcers
Joint (44–70%): symmetric, migratory
arthralgias
of small or medium joints
Renal (50%):
glomerulonephritis
(proteinuria, hematuria, ARF, HTN, edema)
Neurologic (17–60%):
peripheral neuropathy
(polyneuropathy > mononeuritis multiplex)
Hematologic: anemia, thrombocytopenia, ↑ risk of B-cell lymphoma
GI (5%): abdominal pain, hepatosplenomegaly, abnormal LFTs
Diagnostic studies
• ✓ Cryoglobulins; must keep blood warmed to 37°C at all times en route to lab; early cooling causes falsecryoglobulin, loss of RF and ↓↓ complement • Cryocrit is quantification of cryoprotein, does not always correlate w/ disease activity • False ↑ in WBC or plt on automated CBC, due to cryoprecipitation
• Type I: ✓ serum viscosity, symptomatic if ≥4.0 centipoise; complement levels normal • Type II: ↓
C4 levels
, variable C3 levels, ↑ ESR,rheumatoid factor (RF) ✓
HCV, HBV, & HIV serologies
in all Pts w/ mixed cryoglobulinemia Bx of affected tissue: hyaline thrombi; vasculitis w/ mixed inflammatory infiltrates of small vessels; leukocytoclastic vasculitis in purpuric lesions
Treatment
(Autoimmun Rev 2011;10:444; Arth Rheum 2012;64:604; Blood 2012;119:5996)
•
Treat underlying disorder
:
Lymphoproliferative disease: chemotherapy and/or radiation
HCV: antivirals ± immunosuppression for severe disease
Connective tissue-related disease: DMARD/steroids ± rituximab
• Type I: Plasma exchange if hyperviscosity
• Type II: NSAIDs for control of mild symptoms for Pts w/ normal renal function
Rituximab or cyclophosphamide for major organ involvement
Plasmapheresis or plasma exchange in severe, life-threatening disease
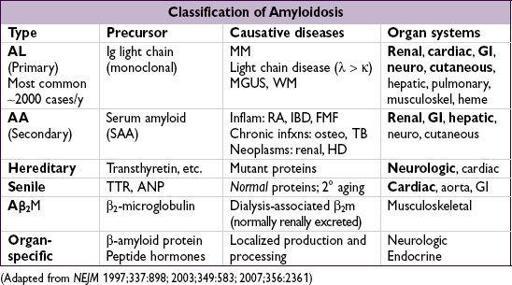
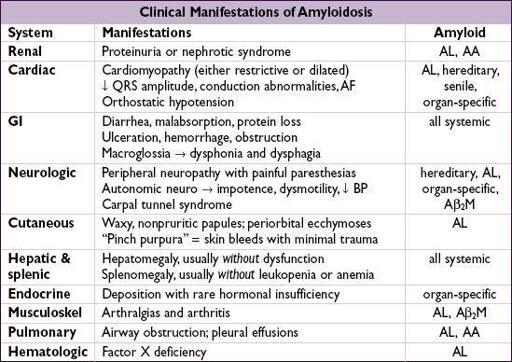
AMYLOIDOSIS
The deposition of misfolded and insoluble fibrous proteins in normal organs and tissues.
Diagnostic studies
• If suspect AL → ✓ SIEP & UIEP (↑ Se vs. SPEP & UPEP) & free light chains, ± BM bx • If suspect renal involvement ✓ U/A (proteinuria)
• If suspect cardiac involvement: ✓ ECG (↓ voltage, conduction abnl), echo (biventricular thickening with “granular sparkling” appearance; ↑ wall w/o ↑ volt 75% Se, 95% Sp), MRI • Biopsy (abdominal SC fat pad, rectal or affected tissue) → apple-green birefringence on
Congo red stain
; fat pad bx Se 60–85%, Sp 90–100%
• Genetic testing for hereditary forms
Treatment
• AL: ? high-dose melphalan → auto HSCT if limited organ dysfxn (NEJM 2007;357:1083); o/w low-dose melphalan + dexamethasone; novel agents (eg, bortezomib, lenalidomide, thalidomide) being evaluated (J Hematol Oncol 2011;4:47) • AA: Rx underlying disease; colchicine for FMF esp. to prevent progressive renal disease (NEJM 2007;356:23); eprodisate promising for renal disease (NEJM 2007;356:2349) • For hereditary amyloidoses in which amyloid precursor protein is produced by the
liver (eg, TTR), liver transplantation may prevent further deposition
• Cardiac involv.: diuretics; avoid dig & CCB; avoid vasodilators; ? ICD for 1° prevention • Heart, kidney and liver Tx may be considered in those w/ advanced disease
Prognosis
• AL amyloid: median survival ~12–18 mo; if cardiac involvement, median survival ~6 mo • AA amyloid: median survival ~11 y (NEJM 2007;356:2361)
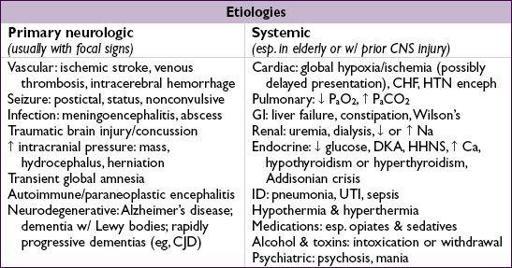
CHANGE IN MENTAL STATUS
Definitions (description of patient & timing is most helpful)
•
Unresponsive
: implies ↓ arousal or ability to follow commands, specify w/ exam
•
Delirium
(aka acute confusional state or encephalopathy): acute change in attention and consciousness with fluctuations. May include sleep–wake dysregulation, autonomic changes, abnormal sensory perception and changes in affect as additional features.
•
Dementia:
impaired cognition, often incl. memory. Usually chronic & progressive, eventually encompassing more anatomical & functional parts of the nervous system.
Initial evaluation
•
History
(witness & background
crucial
): time course, previous illnesses including dementia or psych; head trauma; meds, drug/alcohol use; infection/immune status
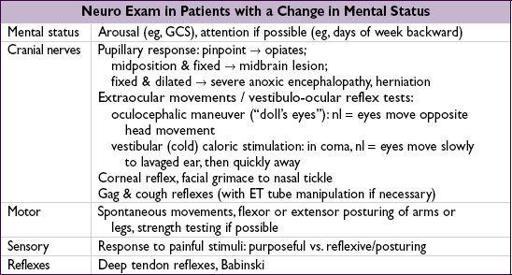
•
General physical exam
:
vital signs
, signs of trauma, asterixis, stigmata of liver disease, embolic phenomena, signs of drug use, nuchal rigidity (may be present in meningitis or SAH, but
do not test
if possible trauma/cervical spine fracture)
•
Neurologic exam
(most meaningful off sedatives/paralytics): look for focality or s/s of ↑ ICP (eg, HA, vomiting, papilledema, unilateral dilated pupil, ↑ BP)
Other books
Unsafe Harbor by Jessica Speart
the Rider Of Ruby Hills (1986) by L'amour, Louis
Not Quite Mine (Not Quite series) by Bybee, Catherine
This Charming Man by Keyes, Marian
Soaked (The Water's Edge #2) by Stacy Kestwick
Knight Defender (Knight Chronicles) by Rue Allyn
Arrow’s Flight by Mercedes Lackey
Temptation by Leda Swann
The Avenger 15 - House of Death by Kenneth Robeson
Twice As Nice by Lin Oliver