Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (56 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

however
, above assumes entire infusate retained
without any output of Na or H
2
O if Pt euvolemic, as in SIADH, infused Na will be excreted eg, 1 L NS (154 mEq of Na or 308 mOsm of solute in 1 L free H
2
O) given to Pt with SIADH with U
osm
= 616 → 308 mOsm solute excreted in 0.5 L H
2
O → net gain 0.5 L H
2
O → ↓ [Na]
serum
∴ normal saline can
worsen
hyponatremia 2° SIADH if U
osm
> infusate
osm
•
Hypovolemic hyponatremia
: volume repletion with normal saline at a
slow rate
. Once volume replete → stimulus for ADH removed → kidneys excrete free H
2
O → serum Na will correct very rapidly (D
5
W ± ddAVP if overcorrection) (
KI
2009;76:587).
•
SIADH
(
NEJM
2007;356:2064):
free water restrict
+ treat underlying cause
hypertonic saline
(± loop diuretic) if sx or Na fails to ↑ w/ free H
2
O restriction 1 L hypertonic saline (3% NaCl) will raise [Na]
serum
by ~10 mEq (see above) ~50 mL/h will ↑ [Na] by ~0.5 mEq/L/h; 100–200 mL/h will ↑ [Na] by ~1–2 mEq/L/h formula only provides estimate; ∴ recheck serum Na frequently (at least q2h)
salt tabs: particularly if chronic and no CHF
aquaresis: conivaptan (IV V1a & V2 vasopressin receptor antag) or tolvaptan (oral V2 antag;
NEJM
2006;355:2099); used for symptomatic SIADH resistant to above Rx but rate of correction can be rapid (
AJKD
2010;56:325)
demeclocycline: causes nephrogenic DI, ↓ U
osm
•
Hypervolemic hyponatremia
:
free water restrict
mobilize excess Na & H
2
O (use loop diuretics; avoid thiazides) & ↑ EAV (vasodilators to ↑ CO in CHF, colloid infusion in cirrhosis)
aquaresis: tolvaptan effective and safe, however no proven mortality benefit, hypoNa recurs after stopping drug, expensive and must monitor for overcorrection (
JASN
2010;21:705;
J Hepatol
2012;56:571)
HYPERNATREMIA
Pathophysiology
(
NEJM
2000;342:1493)
• Deficit of water relative to sodium; by definition, all hypernatremic Pts are hypertonic • Usually
loss of hypotonic fluid
(ie “dehydration”); occasionally infusion of hypertonic fluid •
And
impaired access to free water
(eg, intubation, Δ MS, elderly): hypernatremia is a powerful thirst stimulus, ∴ usually only develops in Pts w/o access to H
2
O
Workup
• ✓ U
osm
, U
Na
, volume status (vital signs, orthostatics, JVP, skin turgor, BUN, Cr)
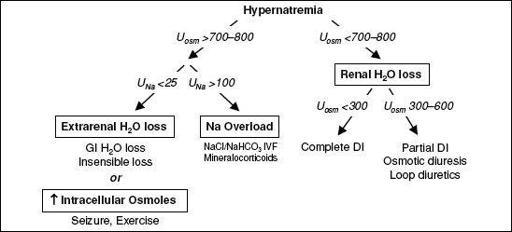
Figure 4-5
Approach to hypernatremia
Extrarenal H
2
O loss (U
osm
>700–800)
•
GI H
2
O loss
: vomiting, NGT drainage, osmotic diarrhea, fistula •
Insensible loss
: fever, exercise, ventilation
Renal H
2
O loss (U
osm
<700–800)
•
Diuresis
: osmotic (glc, mannitol, urea), loop diuretics •
Diabetes insipidus
(
J Clin Endocrinol Metab
2012;97:3426)
ADH deficiency (central) or resistance (nephrogenic)
Central
: hypothalamic or posterior pituitary disease (congenital, trauma/surgery, tumors, infiltrative/IgG4); also idiopathic, hypoxic encephalopathy, anorexia, EtOH
Nephrogenic
(
Annals
2006;144:186)
congenital (ADH receptor V2 mutation, aquaporin-2 mutation;
Pediatr Nephrol
2012;27:2183)
drugs:
lithium
, amphotericin, demeclocycline, foscarnet, cidofovir metabolic:
hypercalcemia
,
severe hypokalemia
, protein malnutrition, congenital tubulointerstitial:
postobstruction
,
recovery phase of ATN
, PKD, sickle cell, Sjögren’s, amyloid, pregnancy (placental vasopressinase)
DI usually presents as
severe polyuria
and
mild hypernatremia
Other
(U
osm
>700–800)
•
Na overload
: hypertonic saline (eg, resuscitation w/ NaHCO
3
), mineralocorticoid excess •
Seizures
,
≠ exercise
: ↑ intracellular osmoles → H
2
O shifts → transient ↑ [Na]
serum
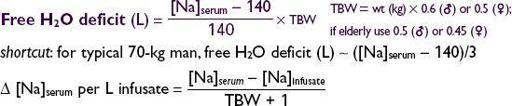
Treatment
•
Restore access to H
2
O
or supply daily requirement of H
2
O (≥1 L/d) •
Replace free H
2
O deficit
(also replace concurrent volume deficit if appropriate):
eg, 1 L D
5
W given to 70-kg man w/ [Na] = 160 mEq/L will ↓ [Na]
serum
by 3.7 mEq •
Rate of Ø of Na should not exceed 0.5 mEq/L/h
to avoid cerebral edema
shortcut
: in 70-kg man, 125 mL/h of free H
2
O will ↓ [Na] by ~0.5 mEq/L/h •
1
/
2
NS (77 mEq/L) or
1
/
4
NS (38 mEq/L) provides both volume & free H
2
O (500 or 750 mL of free H
2
O per L, respectively); can give free H
2
O via NGT/OGT
• Formulas provide only estimates; ∴ recheck serum Na frequently •
DI and osmotic diuresis
: see “Polyuria” section below •
Na overload
: D
5
W + diuretic
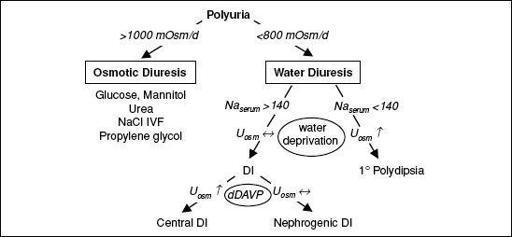
POLYURIA
Definition and pathophysiology
•
Polyuria
defined as >3 L UOP per day • Due to an
osmotic
or a
water diuresis
; almost always due to osmotic diuresis in inpatients
Workup
• Perform a timed urine collection (6 h sufficient) and measure U
osm
• 24-h osmole excretion rate = 24-h UOP (actual or estimate) × U
osm
>1000 mOsm/d → osmotic diuresis
<800 mOsm/d → water diuresis
Osmotic diuresis
• Etiologies
Glucose (uncontrolled diabetes mellitus)
Mannitol
Urea: recovering ARF, ↑ protein feeds, hypercatabolism (burns, steroids), GI bleed
NaCl administration
Propylene glycol
Water diuresis
• Etiologies:
diabetes insipidus
(DI) (Na
serum
>140) or
1
°
polydipsia
(Na
serum
<140) see “Hypernatremia” above for list of causes of central and nephrogenic DI • Workup of DI: U
osm
<300 (complete) or 300–600 (partial)
water deprivation test
(start in a.m., ✓ Na
serum
, P
osm
, U
osm
, UOP q1–2h)
Deprive until P
osm
>295, then ✓ U
osm
. If U
osm
<300, then administer vasopressin (5 U SC) or dDAVP (10 µg intranasal), then check U
osm
in 1–2 h: U
osm
↑ by >50% = central DI U
osm
unchanged = nephrogenic DI
✓ ADH level before and after water deprivation to evaluate proper response
Figure 4-6 Approach to polyuria
Treatment
•
1º polydipsia
: treat psychiatric illness, check meds, restrict access to free H
2
O
•
Osmotic diuresis
: address underlying cause, replace free H
2
O deficit (see “Hypernatremia” for formula to calculate) and ongoing losses •
DI
: