Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (114 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
8.61Mb size Format: txt, pdf, ePub
biopsy → microgranulomas, fibrinoid necrosis and thrombosis of small arteries and
veins with eosinophilic infiltrates
• Treatment: high-dose
corticosteroids
+ cyclophosphamide if severe
Renal-limited vasculitis
• Small vessel pauci-immune vasculitis causing RPGN w/o other organ involvement • Dx studies: 80%ANCA (MPO > PR3); biopsy with pauci-immune GN ± granulomas • Treatment identical to that for GPA/MPA
IMMUNE COMPLEX–ASSOCIATED SMALL-VESSEL VASCULITIS
Henoch-Schönlein purpura (HSP)
•
IgA-mediated
vasculitis w/ predilection for
skin
,
GI tract
and
kidneys
• Epidemiology:>
, children > adults, onset in winter > summer • May develop after upper respiratory tract infection (esp. strep) or drug exposure • Clinical manifestations
palpable purpura
on extensor surfaces (lower extremity first) & buttocks
polyarthralgias
(nondeforming) esp. involving hips, knees, & ankles
colicky
abdominal pain
± GIB or intussusception
nephritis ranging from
microscopic hematuria
& proteinuria to ESRD
• Dx studies:
skin bx w/ immunofluorescence
→
leukocytoclastic vasculitis
w/
IgA
and
C3
deposition in vessel wall; renal bx → mesangial IgA deposition
• Treatment: often self-limiting over 4 wk; steroids ± DMARDs for renal or severe disease
Cryoglobulinemic vasculitis (see “Cryoglobulinemia”)
Connective tissue disease–associated vasculitis
• Small vessel vasculitis a/w
RA
,
SLE
or
Sjögren’s syndrome
• Clinical manifestations
distal arteritis: digital ischemia, livedo reticularis, palpable purpura, cutaneous ulceration
visceral arteritis: pericarditis and mesenteric ischemia
peripheral neuropathy
• Dx studies: skin/sural nerve bx, angiography, EMG; ↓ C′ in SLE;RF or anti-CCP in RA • Treatment: steroids, cyclophosphamide, MTX (other DMARDs)
Cutaneous leukocytoclastic angiitis
• Heterogeneous group of clinical syndromes due to
immune complex deposition
in capillaries, venules and arterioles; includes
hypersensitivity vasculitis
• Overall the most common type of vasculitis • Etiologies
drugs: PCN, ASA, amphetamines, levamisole, thiazides, chemicals, immunizations
infections: Strep, Staph, endocarditis, TB, hepatitis
malignancy (paraneoplastic)
• Clinical manifestations: abrupt onset of
palpable purpura
and
transient arthralgias
after exposure to the offending agent; visceral involvement rare but can be severe • Dx studies: ↑ ESR, ↓ complement levels, eosinophilia; ✓ U/A;
skin biopsy
→ leukocytoclastic vasculitis
w/o
IgA deposition
in skin (to distinguish from HSP); if etiology not clear, consider ANCA, cryoglobulins, hepatitis serologies, ANA, RF
• Treatment: withdrawal of offending agent ± rapid prednisone taper
Behçet’s syndrome
(
Curr Rheum Opin
2010;12:429)
•
Systemic vasculitis
affecting all vessel sizes, a/w
oral and/or genital ulcers
• Epidemiology: usually young adults (25–35 y); a/w HLA-B51 in areas of highest prevalence on the old Silk Road (Turkey, Middle East and other Asian countries) • Classification criteria (#1 + ≥2 others is 91% Se & 96% Sp; Lancet 1990;335:1078) 1. recurrent
oral aphthous ulceration
(≥3× in 1 y, usually 1st manifestation) 2. recurrent
genital ulceration
(labia in females, scrotum in males) 3.
eye
lesions: uveitis, scleritis, retinal vasculitis, optic neuritis (may threaten vision) 4.
skin
lesions: pustules, papules, folliculitis, erythema nodosum (scarring) 5.pathergy test (prick forearm w/sterile needle → pustule) (not sensitive in Caucasians) • Other clinical manifestations: most recur but are not chronic
arthritis: mild, ± symmetric, nondestructive, involving knees and ankles
neurologic: usually involvement of midbrain parenchyma; peripheral neuropathy rare
vascular: superficial or deep vein thrombosis (25%); arterial stenosis, occlusion and aneurysm can also occur; low incidence of thromboembolism
• Dx studies: ↑ ESR/CRP; ulcer swab to r/o HSV; ulcer bx nonspecific; ophtho eval if sx • Treatment (Rheumatology 2007;46:736; Ann Rheum Dis 2008;67:1656 & 2009;68:1528)
mucocutaneous
mild:
topical steroids
,
colchicine
(esp. for erythema nodosum), dapsone
severe: oral steroids, steroid-sparing agents
arthritis: NSAIDs, colchicine, steroids, steroid-sparing agents
ocular:
topical and/or systemic steroids
± steroid-sparing agents
steroid-sparing: AZA, anti-TNF, CYC (large vessel and CNS ds), CsA, MTX, IFNɑ-2A
venous thrombosis: steroids and anticoagulation (careful if aneurysm present)
IGG4-RELATED DISEASE
Definition & etiology
(
NEJM 2012;366:539)
• Responsible for
tumor-like inflammatory lesions
of nearly every organ/tissue • Etiology unclear: ? autoimmune; unclear role of IgG4 Ab; may have h/o atopy
Clinical manifestations
• Commonly pancreatitis, aortitis, cholangitis, sialadenitis, orbital structures, retroperitoneal fibrosis • Multiple lesions may be present synchronously or metachronously
Diagnosis
(Mod Pathol 2012;25:1181)
•
Biopsy
w/ specific histopathology & immunohistochemistry findings: lymphoplasmacytic infiltrate w/ significant IgG4+ plasma cell infiltrate, fibrosis, obliterative phlebitis • ↑ serum IgG4 in 40%; not specific seen in GPA, bronchiectasis, etc (Modern Rheum 2012;22:419)
Treatment
•
Prednisone
vs. rituximab (Medicine 2012;91:57)
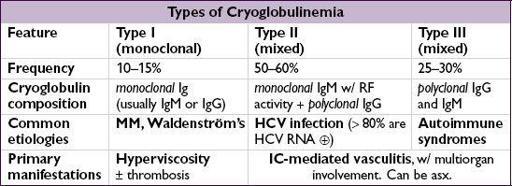
CRYOGLOBULINEMIA
Definition & types
(Lancet 2012;379:348)
•
Proteins that precipitate on exposure to the cold and redissolve on rewarming
, characterized by their composition •
Cryoglobulins
=proteins that precipitate from serum and plasma when cooled • Distinguish from cryo
fibrinogenemia
=proteins (eg, fibrin, fibrinogen) that precipitate only from plasma; found in autoimmune dis, malignancies, infxns; unclear clinical significance
Other books
Swim the Fly by Don Calame
The Wives of Beverly Row 1: Lust Has a New Address by Weeks, Abby
2041 Sanctuary (Dark Descent) by Robert Storey
Blood Sacrifice by By Rick R. Reed
A Beginner's Guide to Rakes by Suzanne Enoch
Living As a Moon by Owen Marshall
The Duke's Agent by Rebecca Jenkins
The Dark: A Collection (Point Horror) by Cargill, Linda
Rewired (The Progress Series) by Queau, Amy
A Man Called Ove by Fredrik Backman