Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (112 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

VASCULITIS
OVERVIEW
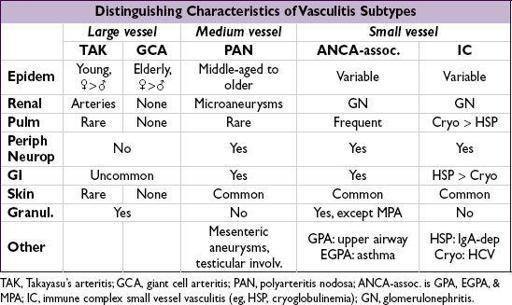
• Inflammation w/in blood vessel walls causing end-organ damage often a/w systemic sx; may be primary or secondary (eg, infection, malignancy) in etiology • Classified by size of predominant vessel affected (Arthritis Rheum 2013;65:1); overlap of vessel size affected is common • Clinical manifestations based on size of vessels involved; constitutional sx (low-grade fever, fatigue, weight loss, myalgias, anorexia) common to all
LARGE-VESSEL VASCULITIS
Takayasu’s arteritis
(“pulseless disease”)
•
Arteritis of aorta and its branches
→
stenosis/aneurysm
→ claudication; onset <50 y • Pattern of involvement: aorta and branches; most often
subclavian
and
innominate arteries
(>90%), as well as carotid, coronary, renal, pulmonary (~50%) • Epidemiology: Most common in
Asia
; :
: ~9:1;
~9:1;
age <50 y
• Clinical manifestations and physical findings
Systemic inflamm with
fever
,
arthralgias
, wt loss
Vessel inflamm w/ pain & tenderness, ↓
& unequal pulses/BPs in extremities
,
bruits
, limb claudication, renovascular HTN (>50%), neurogenic syncope; Ao aneurysm ± AI
“Burnt out” or fibrotic period (eg, vascular stenosis)
• Dx studies: ↑ ESR (75%), CRP;
arteriography
→ occlusion, stenosis, irregularity and aneurysms; carotid U/S Doppler studies; PET-CT; MRA;
pathology
→ focal panarteritis, cellular infiltrate with granulomas and giant cells (bx not required for dx) • Treatment:
steroids
± MTX or AZA; anti-TNF (2nd line, Autoimmun Rev 2012;11:678), ASA, surgical/endovascular revasc (Circ 2008;69:70) • Monitoring: MRA or PET-CT (Arth Rheum 2012;64:866); ESR/CRP (Ann Rheum Dis 2009;68:318)
Giant cell arteritis (GCA)
(
Curr Rheumatol Rep
2010;12:436)
•
Granulomatous arteritis of aorta/branches
w/ predilection for
temporal artery
, a/w PMR, onset >50 y • Pattern of involvement:
extracranial branches of carotid artery
, esp. temporal artery (thus also called
temporal arteritis
); aorta and/or its branches in 10–80%
• Epidemiology: 90% of Pts >60 y, extremely rare <50 y;:
=3:1
• Clinical manifestations (JAMA 2002;287:92)
constitutional sx:
fevers
,
fatigue
, wt loss, PMR sx (see below)
temporal artery (TA)
→
headache, tender TAs
and scalp; absent TA pulse
ophthalmic artery (20%) → optic neuritis, diplopia, amaurosis fugax, blindness
facial arteries →
jaw claudication
large vessel vasculitis → intermittent claudication of extremities; thoracic Ao aneurysm
• Dx studies: ↑
ESR
(ESR <40 in ~5%), ↑ CRP, anemia
(ESR related to fibrinogen & Ig in blood; Ddx for >100: malignancy esp. multiple myeloma, lymphoma; GCA or other vasculitis; ESRD; endocarditis, TB, osteomyelitis)
temporal artery bx
whenever GCA
suspected
(Se ≤85%); 1–2 cm ± bilat to ↑ yield (3–7% discordance) (Ann Rheum Dis 2009;68:318) → vasculitis & granulomas
if suspect aortitis or lg vessel involvement (BP Δ or bruits) → MRI/MRA or PET-CT
•
Polymyalgia rheumatica
(Lancet 2013;381:63)
seen in 50% of GCA Pts; 15% of Pts w/ PMR develop GCA
age ≥50 y; ESR >40 mm/h (and/or ↑ CRP); bilateral
pain & morning stiffness
(>30 min × ≥1 mo), involving 2 of 3 areas: neck or torso, shoulders or prox. arms, hips or prox. thighs; nighttime pain; exclude other causes of sx (eg, RA); nl CK
• Rx:
steroids
(do not await bx/path results to begin steroids, have at least 2 wk to bx)
GCA: 40–60 mg/d w/
slow
taper, ASA daily; consider IV pulse if vision threatened
PMR:10–20 mg/d (Semin Arthritis Rheum 2007;37:13)
• Monitoring: follow clinical status & ESR/CRP (Ann Rheum Dis 2009;68:318)
MEDIUM-VESSEL VASCULITIS
Polyarteritis nodosa
(“classic” PAN) (
Arth Rheum
2010;62:616)
•
Necrotizing nongranulomatous vasculitis of medium and small arteries
(w/ muscular media) w/o glomerulonephritis or capillary involvement (ie, DAH), not a/w ANCA • Epidemiology: >
> ; average age of onset ~50 y; primary or
; average age of onset ~50 y; primary or
HBV-associated
(~10%) • Clinical manifestations
constitutional sx (80%): wt loss,
fever
, fatigue
neuro (79%):
mononeuritis multiplex
, peripheral neuropathies, stroke
musculoskeletal (64%):
extremity pain
, myalgias, arthralgias, arthritis
renal (51%):
HTN
, hematuria, proteinuria, renal failure, glomerulonephritis unusual
GI (38%):
abd pain
, GIB/infarction, cholecystitis; GU (25%): ovarian or testicular pain
skin (50%):
livedo reticularis
, purpura, nodules, ulcers, Raynaud’s
ophthalmic (9%): retinal vasculitis, retinal exudates, conjunctivitis, uveitis
cardiac (22%): coronary arteritis, cardiomyopathy, pericarditis
if lung involvement, suspect other vasculitis
• Dx studies: ↑ ESR/CRP,ANCA; ✓ HBs Ag; ↓ C3/C4 if HBV-associated