Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (95 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

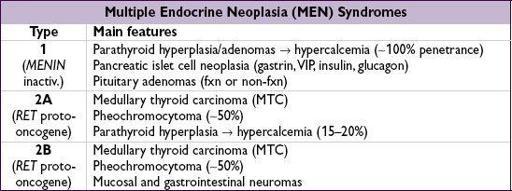
HYPERPITUITARY SYNDROMES
Pituitary tumors
• Pathophysiology: adenoma → excess of trophic hormone (if tumor fxnal, but 30–40% not) and potentially
deficiencies
in other trophic hormones due to compression; cosecretion of PRL and growth hormone in 10% of prolactinomas • Clinical manifestations: syndromes due to oversecretion of hormones (see below)
± mass effect: headache, visual Ds, diplopia, cranial neuropathies
• Workup: MRI, hormone levels, ± visual field testing, consider MEN1 (see below)
if <10 mm, mass effect, no hormonal effects, can f/up q3–6mo
Hyperprolactinemia
(
NEJM
2010;362:1219)
• Etiology
prolactinoma (50% of pituitary adenomas)
stalk compression due to nonprolactinoma → ↓ inhibitory dopamine → ↑ PRL (mild)
• Physiology: PRL induces lactation and inhibits GnRH → ↓ FSH & LH
• Clinical manifestations:
amenorrhea
,
galactorrhea
,
infertility
, ↓ libido, impotence • Diagnostic studies: ↑
PRL
(✓
fasting
levels), but elevated in many situations, ∴ r/o pregnancy or exogenous estrogens, hypothyroidism, dopamine agonists (psych meds, antiemetics), renal failure (↓ clearance), cirrhosis, stress, ↑ carb diet.
MRI
to evaluate for tumor; visual field testing if MRI shows compression of optic chiasm.
• Treatment
If asx (no HA, galactorrhea, hypogonadal sx) & microadenoma (
<10 mm
), follow w/ MRI
If sx or macroadenoma (
≥10 mm
) options include:
medical
with dopamine agonist such as cabergoline (70–100% success rate) or bromocriptine (not as well tol); side effects include N/V, orthostasis, nasal congestion, tricuspid valve regurgitation (✓ echo before & q1–2y during Rx) (
JCEM
2010:95:1025)
surgical:
transsphenoidal surgery (main indications: failed or cannot tolerate medical Rx, GH cosecretion or neurologic sx not improving); 10–20% recurrence rate
radiation:
if medical or surgical therapy have failed or are not tolerated
Acromegaly
(↑ GH; 10% of adenomas;
NEJM
2006;355:2558)
• Physiology: stimulates secretion of insulin-like growth factor 1 (IGF-1) • Clinical manifestations: ↑ soft tissue, arthralgias, jaw enlargement, headache, carpal tunnel syndrome, macroglossia, hoarseness, sleep apnea, amenorrhea, impotence, diabetes mellitus, acanthosis/skin tags, ↑ sweating, HTN/CMP, colonic polyps • Diagnostic studies:
no utility in checking random GH levels because of pulsatile secretion
≠ IGF-
1 (somatomedin C); ± ↑ PRL; OGTT → GH
not
suppressed to <1 (<0.3 if newer assay) ng/mL; pituitary MRI to evaluate for tumor
• Treatment:
surgery
, octreotide (long-and short-acting preparations), dopamine agonists (if PRL cosecretion), pegvisomant (GH receptor antagonist), radiation • Prognosis: w/o Rx 2–3× ↑ mortality, risk of pituitary insufficiency, colon cancer
Cushing’s disease
(↑ ACTH)
: 10–15% of adenomas; see “Adrenal Disorders”
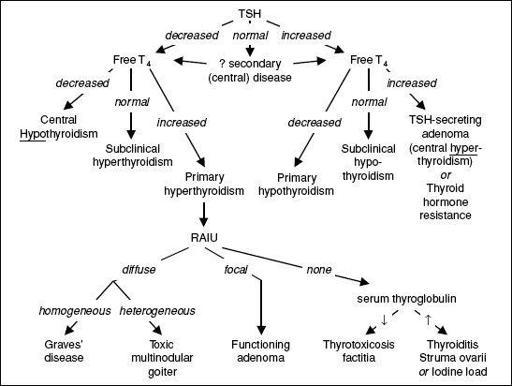
Central hyperthyroidism
(↑ TSH, ↑ ɑ-subunit)
: extremely rare; see “Thyroid Disorders”
↑ FSH & LH
: usually non-fxn, presents as
hypopituitarism
b/c of compression effects
THYROID DISORDERS
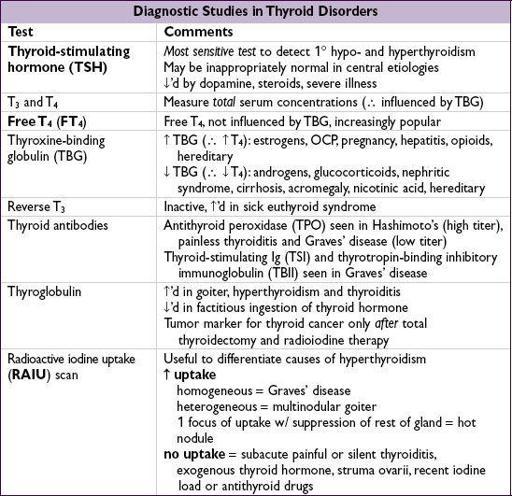
Figure 7-1 Approach to thyroid disorders
HYPOTHYROIDISM
Etiologies
• Primary (>90% of cases of hypothyroidism; ↓
free T
4
, ↑ TSH)
Goitrous:
Hashimoto’s thyroiditis
, after hyperthyroid phase of thyroiditis, iodine defic, Li, amiodarone
Nongoitrous: surgical destruction, s/p radioactive iodine or XRT, amiodarone
• Central (↓ free T
4
, low/nl or slightly high TSH): hypothalamic or pituitary failure (TSH levels ↓ or “normal,” can be slightly ↑ although functionally inactive due to abnormal glycosylation)
Hashimoto’s thyroiditis
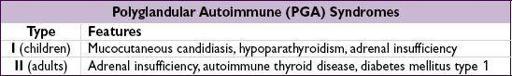
• Autoimmune destruction with patchy lymphocytic infiltration • Associated with other autoimmune disease and may be part of PGA syndrome type II •antithyroid peroxidase (anti-TPO) and antithyroglobulin (anti-Tg) Abs in >90%
Clinical manifestations
(
Annals
2009;151:ITC61)
•
Early
: weakness, fatigue, arthralgias, myalgias, headache, depression, cold intolerance, weight gain, constipation, menorrhagia, dry skin, coarse brittle hair, brittle nails, carpal tunnel syndrome, delayed DTRs (“hung up” reflexes), diastolic HTN, hyperlipidemia •
Late
: slow speech, hoarseness, loss of outer third of eyebrows,
myxedema
(nonpitting skin thickening due to↑ glycosaminoglycans), periorbital puffiness, bradycardia, pleural, pericardial, & peritoneal effusions, atherosclerosis •
Myxedema crisis
: hypothermia, hypotension, hypoventilation, Δ MS (including coma) hyponatremia, hypoglycemia; often precipitated by infection or major cardiopulmonary or neurologic illness (
Med Clin North Am
2012;96:385)
Diagnostic studies
• ↓
FT
4
; ↑
TSH
in primary hypothyroidism;antithyroid Ab in Hashimoto’s thyroiditis • May see hyponatremia, hypoglycemia, anemia, ↑ LDL, ↓ HDL and ↑ CK
• Screening recommended for pregnant women
Treatment of overt hypothyroidism
• Levothyroxine (1.5–1.7 µg/kg/d), re ✓ TSH q5–6wk and titrate until euthyroid;
sx can take mos to resolve;
lower starting dose
(0.3–0.5 µg/kg/d) if at risk for ischemic heart disease or elderly; advise Pt to keep same formulation of levothyroxine
↑
dose
typically needed if: pregnancy (~30% ↑ by wk 8), initiation of estrogen replacement, on meds that accelerate T
4
catabolism (eg, phenytoin, phenobarbital), poor GI absorption (concomitant Fe or Ca suppl, PPI, sucralfate, cholestyramine, celiac disease, IBD)
• Myxedema coma: load 5–8 µg/kg T
4
IV, then 50–100 µg IV qd; b/c peripheral conversion impaired, may also give 5–10 µg T
3
IV q8h if unstable w/ bradycardia and/or hypothermia (T
3
more arrhythmogenic); must give empiric
adrenal replacement therapy
first as ↓ adrenal reserves in myxedema coma
Subclinical hypothyroidism
(
Lancet
2012;379:1142)
• Mild ↑ TSH and
normal free T
4
with only subtle or no sx • If TSH <7 oranti-TPO Ab, ~
1
⁄
2
euthyroid after 2 y (
JCEM
2012;97:1962) if ↑ titers of antithyroid Abs, progression to overt hypothyroidism is ~4%/y • Rx controversial: follow expectantly or treat to improve mild sx or dyslipidemia most initiate Rx if TSH >10 mU/L, goiter, pregnancy or infertility if TSH 5–10 mU/L Rx if ≤60 y (usually don’t Rx if ≥60 b/c ↑ risk CV complications)