Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (68 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

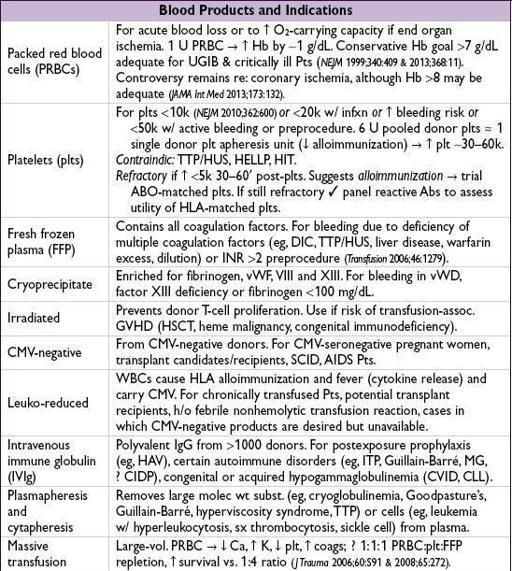
TRANSFUSION THERAPY
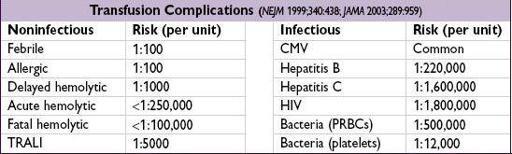
Transfusion reactions
• For all reactions (except minor allergic):
stop transfusion
; send remaining blood product and fresh blood sample to blood bank •
Acute hemolytic
: fever, hypotension, flank pain, renal failure <24 h after transfusion
Due to ABO incompatibility → preformed Abs against donor RBCs
Treatment: vigorous IVF, maintain UOP with diuretics, mannitol or dopamine
•
Delayed hemolytic
: generally less severe than acute hemolytic; 5–7 d after transfusion
Due to undetected allo-Abs against minor antigens → anamnestic response
Treatment: usually no specific therapy required; dx is important for future transfusion
•
Febrile nonhemolytic
: fever and rigors 0–6 h after transfusion
Due to Abs against donor WBCs and cytokines released from cells in blood product
Treatment: acetaminophen ± meperidine; r/o infection and hemolysis
•
Allergic
: urticaria; rarely,
anaphylaxis
: bronchospasm, laryngeal edema, hypotension Reaction to transfused proteins; anaphylaxis seen in IgA-deficient Pts w/ anti-IgA Abs
Treatment: urticaria → diphenhydramine; anaphylaxis → epinephrine ± glucocorticoids
•
Transfusion-related acute lung injury
(TRALI): noncardiogenic pulmonary edema Due to donor Abs that bind recipient WBCs, which then aggregate in pulmonary vasculature and release mediators causing ↑ capillary permeability Treatment: see “ARDS”
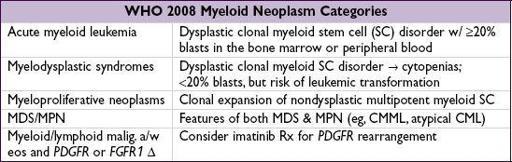
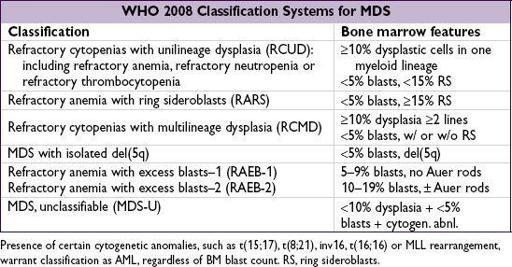
MYELODYSPLASTIC SYNDROMES (MDS)
Myeloid neoplasm overview
(
Blood
2009;114:937)
• 5 categories based on BM morphology, clinical characteristics and genetics
Myelodysplastic syndromes (MDS) overview
(
NEJM
2009;361:1872)
• Acquired clonal stem cell disorder → ineffective hematopoiesis →
cytopenias
,
dysmorphic blood cells and precursors
, variable risk of
leukemic transformation
• Epidemiology: >10,000 cases/y; median age ~65 y; male predominance (1.8×) •
Idiopathic
or 2° to chemo w/
alkylating agents
; ↑ risk w/ radiation, benzene • Clinical manifestations:
anemia
(85%), neutropenia (50%), thrombocytopenia (40–65%) • Diagnosis: dysplasia (usually multilineage) in peripheral smear (ovalomacrocytes,
pseudo-Pelger-Huët anomaly
) and bone marrow (≥10% dysplasia with blasts ± RS) • Both
cytogenetic
[eg, del(5q), mono 7, del(7q), trisomy 8, del(20q)] and
molec
abnl (eg, TP53, EZH2, ETV6, RUNX1, ASXL1, SF3B1) have prognostic signif (
NEJM
2011;364:2496) • Prior to dx MDS: exclude AML (≥20% blasts) and CMML (monocyte count >1 × 10
9
/L); r/o 2° BM Ds due to defic. of B
12
, folate, copper; viral infections (eg, HIV); chemotherapy; alcohol abuse; lead or arsenic toxicity
• Rx (
Am J Hematol
2012;87:692): intensity based on IPSS-R (qv), age, performance status (PS)
Poor PS, any risk → supportive care = transfusions, G-CSF, Epo, abx if needed
Low/intermediate risk → Epo (esp. if Epo level <500); lenalidomide (esp. for 5q syndrome;
NEJM
2005;352:549); DNA hypomethylating agents (azacitidine or decitabine)
Intermediate/high risk → DNA hypomethylating agents (survival advantage w/ azacytidine;
Lancet Oncol
2009;10:223), combination
chemo
(akin to AML Rx) or
allogeneic HSCT
if age <55 (consider reduced-intensity transplant for ages 55–75)