Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (59 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

? ↑ diuresis w/ co-administration of albumin if ↓ serum albumin (
Crit Care Med
2005;33:1681)
Thiazide diuretics
(
NEJM
2009;361:2153)
•
Drugs
: hydrochlorothiazide (HCTZ), chlorothiazide (Diuril), metolazone (Zaroxolyn) •
Mechanism
: inhibit Na-Cl cotransporter in the distal convoluted tubule (DCT)
synergistic with loop diuretic
, esp. if chronic loop use
↓ effect when GFR <30,
except metolazone
which is still effective in renal insufficiency
•
Dosing
: give prior to loop diuretic, typically ~30 min before
K-sparing diuretics
•
Drugs
: spironolactone (Aldactone), amiloride, triamterene, eplerenone •
Mechanism
: ↓ Na reabsorption in collecting duct (amiloride/triamterene inhibit principal cell Na channel [ENaC]; spironolactone/eplerenone inhibit mineralocorticoid receptor). Relatively weak natriuretic activity, useful in combination with thiazide or in cirrhosis.
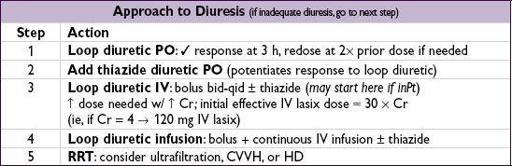
Disease state specific regimens
• Renal insufficiency: loop diuretic (↑ dose to achieve effective delivery to ThAL) ± thiazide • CHF: loop diuretic (↑ frequency over ↑ dose) + thiazide (watch K & Mg) • Nephrotic syndrome: urinary albumin binds secreted loop diuretic, use 2–3 × normal dose • Cirrhosis: spironolactone (blocks 2° hyperaldosteronism) + lasix in 2.5:1 ratio • Severe metabolic alkalosis: acetazolamide & treat underlying cause
Adverse effects
• Loop: ± ↑ Na, ↓ K, ↓ Mg, ↓ Ca, hyperuricemia, ototoxicity, hypersensitivity (sulfa) • Thiazide: ↓ Na, ↓ K, ↓ Mg, ↑ Ca, hyperlipidemia, pancreatitis, ↑ glucose • K-sparing: ↑ K (esp. w/ ACEI), metabolic acidosis, gynecomastia (spironolactone)
RENAL REPLACEMENT AND DIALYSIS
General
• Substitutes for renal solute and fluid removal;
Acute:
CVVH vs. HD;
Chronic:
PD vs. HD
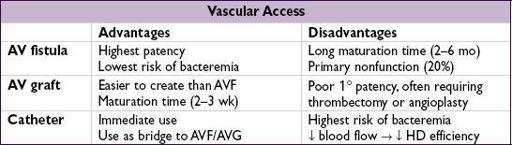
Hemodialysis (HD)
(
NEJM
2010;363:1833)
• Physiology: blood flows along one side of
semipermeable
membrane, dialysate along other
Fluid removal (ie, Na + H
2
O) via transmembrane pressure (TMP) gradient
Solute removal via transmembrane concentration gradient and inversely proportional to size (∴ effective removal of K, urea, and Cr, but not PO
4
)
• Typical orders: duration, volume removal goals, K and Ca in dialysate bath, anticoagulation • 6× vs. 3×/wk improved HTN, LV mass, QoL, but ↑ vasc issues (
NEJM
2010;363:2287); w/ 3×/wk HD, ↑ adverse outcomes after 2 d interval (
NEJM
2011;365:1099) • Complications: HoTN, arrhythmia, access issues (clot, stenosis, infxn, recirculation), disequilibrium syndrome (sx of cerebral edema due to H
2
O shifts after removal of plasma urea during dialysis, esp. in new HD Pts w/ ↑ ↑ BUN), high output HF
• Fever w/ catheter: empiric abx (vanc + AG qHD). GPC > GNR > mixed/fungal. Catheter removal, replacement, or “lock” abx. Consider metastatic infxn w/u (
AJKD
2004;44:779).
Continuous veno-venous hemofiltration (CVVH)
(
NEJM
2012;367:26)
• Physiology:
hemofiltration
rather than dialysis. Blood under pressure passes down one side of
highly permeable
membrane allowing H
2
O and solutes to pass across membrane via TMP gradient (convective clearance). Filtrate discarded. Replacement fluid infused (solute concentrations similar to plasma, except no K, urea, Cr, PO
4
). Fluid balance precisely controlled by adjusting filtrate/replacement fluid.
• Access: double-lumen central venous catheter • Typical orders: volume goals, replacement fluid buffer:
HCO
3
(requires heparin to prevent machine from clotting)
vs. citrate
(hepatically metabolized to HCO
3
; provides anticoagulation w/ in machine via Ca chelation; ∴ requires Ca infusion) • Complications: hypotension, ↓ PO
4
, access complications; ↓ ICa (citrate toxicity in Pts with hepatic dysfunction → look for ↓ ICa but normal/ ↑ serum Ca and AG met acidosis) • Potential advantages over HD: less hypotension, better volume control, removal of inflammatory mediators; however, no survival advantage (
Lancet
2006;368:379) • No advantage for high intensity CVVH over standard intensity (
NEJM
2008;359:7)
Peritoneal dialysis (PD)
(
Perit Dial Int
2001;21:25)
• Physiology: peritoneum acts as membrane. Fluid balance controlled by choosing dialysate [glc] (higher concentrations pull more fluid into peritoneum); longer dwell times pull less fluid as glc equilibrates across peritoneum • Access: permanent catheter inserted in OR
• Typical orders for CAPD (continuous ambulatory peritoneal dialysis):
PD fluid = dextrose (1.5%, 2.5%, or 4.25%), buffer (lactate), Na+, Ca
2
+, Mg
2
+
infuse 10 min, dwell 90 min–5.5 h, drain 20 min
• Can use overnight cycler device that infuses & drains more rapidly, with shorter dwells, while Pt sleeps. Called automated or continuous cycling peritoneal dialysis (APD, CCPD).
• Complications: hypoalbuminemia; right-sided pleural effusion Peritonitis: abd pain, tenderness, cloudy drainage (WBC >100 and >50% PMNs) spectrum: 60–70% GPC, 15–20% GNR, remainder no bacteria or fungal Rx: abx IV or in PD, catheter removal for certain pathogens (eg, yeast,
Pseudomonas
) Hyperglycemia: exacerbated by inflammation, long dwell times, and higher [glc]
Kidney transplantation
(
NEJM
1994;331:365)
• Rx of choice for ESRD; contraindic: active malig, infxn, ischemia, noncompl, subst abuse • Immunosuppression: calcineurin inhib (tacrolimus, CsA), antimetabolite (AZA, MMF), prednisone, ± mTOR inhibitor (sirolimus) (
NEJM
2004;351:2715) • Late renal dysfxn: usual AKI causes + calcineurin tox, rejection, BK virus, recurrence of 1° disease; usual w/u + immunosupp levels, BK virus load, U/S, then bx if no other cause • ↑ risk of infxn (incl opportunistic such CMV, JC, BK viruses) & malignancy (incl PTLD) • ↑ CVD risk due to HTN (calcineurin inhib, RAS), DM & dyslipidemia (immunosupp meds)
GLOMERULAR DISEASE
GLOMERULONEPHRITIS (GN)
Definition
(
NEJM
1998;339:888;
Lancet
2005;365:1797)
•
Pathologically:
intraglomerular inflammation (ranging from focal proliferative [<50% of glomeruli] to diffuse proliferative to crescentic) (
Lancet
2006;368:404) •
Clinically:
hematuria w/ dysmorphic RBCs or RBC casts, ± subnephrotic proteinuria
often w/ renal failure, HTN, edema
•
Progression:
acute GNdays; rapidly progressive GN (RPGN)
wks; chronic GN
mos; can simply have asx hematuria • Crescentic GN (pathologic description)
RPGN (clinical description)