Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (121 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

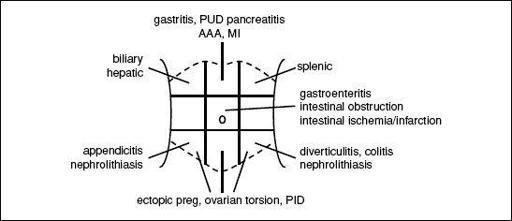
Figure 10-1
Etiologies of abdominal pain based on location
Initial evaluation
• History: onset of pain, location, exacerbating/relieving factors • Assoc. sx: fevers/chills, N/V, Δ in bowel habits (diarrhea/constipation, stool diam. or color, hematochezia, melena), jaundice, Δ in urine color, Δ in wt, menstrual hx in women • PMHx: previous incisions or abdominal surgeries; Ob/Gyn hx
• Exam: VS; general posture of Pt; comprehensive abdominal exam specifically looking for signs of peritonitis, which include rebound tenderness and involuntary guarding, abdominal wall rigidity, pain w/ percussion/minimal palpation; presence of hernias; rectal/pelvic • Labs: CBC, electrolytes, LFTs, amylase/lipase, pregnancy test • Imaging: depends on suspected etiology, may include RUQ U/S for biliary/hepatic disease, KUB for intestinal obstruction, CT for pancreatitis or intestinal disease. Do not delay resucitation or surgical consultation for ill Pt while waiting for imaging.
ACUTE ABDOMEN
Definition
• Acute onset abdominal pain that portends need for urgent surgery
Etiologies
• Perforated viscous → peritonitis (perforated ulcer, complicated diverticulitis, trauma) • Intraperitoneal bleed
• Bowel obstruction (adhesions from previous surgeries, malignancies, hernias) • Mimics: severe pancreatitis can resemble peritonitis; renal colic causes severe abdominal pain but not abdominal rigidity
Initial evaluation
• H&P as above
• Labs as above plus: PT/INR, PTT, type & screen • Imaging: KUB (upright) or if stable, CT abomen/pelvis w/ IV contrast (IV/PO if suspect obstruction)
Initial management
• Immediate surgical consultation for suspected acute abdomen • NPO, start IV fluids (NS or LR)
• Broad spectrum abx if perforation suspected
EXTREMITY EMERGENCIES
Acute limb ischemia
(see “Peripheral Artery Disease” for details)
• Definition: sudden ↓ in perfusion causing threat to limb viability • Evaluation: detailed vascular exam; CT angiography or arteriography • Initial management: anticoag for embolism/thrombosis; immediate surgical consultation
Compartment syndrome
(
Clin Orthop Relat Res
2010;468:940)
• Definition: ↑ intracompartmental pressure w/ compressive closure of venules → ↑ hydrostatic force resulting in further increases in compartment pressure • Etiologies: orthopedic (fracture), vascular (ischemia-reperfusion), iatrogenic (eg, vascular injury in anticoagulated Pt), soft tissue injury (eg, prolonged limb compression) • Clinical manifestations: pain esp. on passive movement, swollen/tense compartment, paraesthesia, pallor, pulselessness, paralysis (late) • Evaluation: ✓ compartment pressures (needle manometry), ICP >30 or difference between diastolic pressure and ICP of >10–30 is diagnostic • Treatment: fasciotomy
SURGICAL TUBES, DRAINS, WOUNDS
Tracheostomy
(
Otolaryngol Head Neck Surg
2013;148:6)
• Inserted either percutaneously or surgically
• Monitor for secretions and suction frequently
• Typically a cuffed tube, which creates a tight seal to facilitate ventilation throught tube
• Speaking valve (eg, Passy-Muir): 1-way valve that allows inhalation through tube, but exhalation around tube through vocal cords (nb, cuff should not be inflated)
• 1st routine tube change for percutaneously placed tubes should be ~10 d postop, whereas surgically placed tubes can be changed >5 d postop and should be overseen by experienced personnel
• Accidental dislodgement of tube:
intubate from above (if airway/vent necessary & anatomically possible)
w/in 7 d of placement: emergent surgical consultation
>7 d after placement: replace with a similar size tube or smaller
Chest tubes
(
Eur J Cardiothorac Surg
2011;40:291)
• Inserted for PTX, chest trauma or after thoracic surgery for drainage of air/ fluid from thoracic cavity. Tubes range from small 10-Fr catheters placed for spontaneous PTX to large bore tubes (28–32 Fr) placed after pulmonary resections.
• Connected to 3-chamber chest drainage system:
1st: collection chamber for pleural fluid
2nd: water seal chamber used to allow air to exit pleural space on exhalation and prevent air from entering on inhalation
3rd: suction control chamber which regulates suction transmitted to pleural space
• Monitor for ouput and presence of air leak (indicated by bubbling in
water seal chamber
)
• Removal determined by overall daily outputs and presence of air leak
• If accidentally removed or dislodged so not functional, tube should be completely removed and an occlusive dressing (eg, 4 × 4 covered w/ Tegederm or silk tape) should be placed
rapidly
over site. CXR STAT; new tube should be placed if persistent PTX.
Gastrostomy/jejunostomy tubes
(
Paediatr Child Health
2011;16:281)
• Placed for tube feedings, hydration and delivery of medications
• Securely anchor to skin to prevent inadvertent removal
• Surrounding skin should be kept dry to prevent breakdown
• Should not be removed for ≥6–8 wk to allow establishment of mature gastrocutaneous tract
• Obstructed tubes can be cleared by flushing with agents such as carbonated water, meat tenderizer, pancreatic enzymes. ↓ obstruction by flushing before & after meds and flushing q4–6h when receiving continuous feeds.
• If becomes inadvertently removed a foley catheter of similar size or smaller should be placed in the tract
immediately
to prevent stoma from closing. Tube then replaced and confirmed via fluoro study w/ gastrograffin.
Suture/staple removal
• Should be done in consultation w/ surgical team
• Timing of removal depends on location of wound: wait 3–4 d before removal from face, 6 d for scalp, 7 d for chest, abdomen & arms, 10 d for back & legs, 14 d for hands
•
Should not be removed if there is evidence of wound separation during removal!
• After removal, wound should be reapproximated w/ steri-strips
MAXIMIZING A SURGICAL CONSULT
• For ill Pt, call surgical consult early, do not wait for labs & imaging results
• If potential surgical emergency, make Pt NPO, start IVF, ✓ coags, type & screen
• Have appropriate-level MD who knows & has examined Pt call consult
OB/GYN ISSUES
VAGINAL BLEEDING
Abnormal bleeding from lower (vulva, vagina, cervix) or upper genital tract (uterus)
Etiologies
• Premenopausal
Not pregnant
: menses, dysfunctional uterine bleeding (menorrhagia), leiomyoma, polyp, trauma, cervical dysplasia/cancer (rare), endometrial hyperplasia/cancer (rare)
Pregnant
1st trimester
: threatened abortion, spont. abortion (missed, incomplete or complete), ectopic pregnancy, molar pregnancy (partial or complete hydatidiform mole)
2nd or 3rd trimester
: preterm labor, placenta previa, placental abruption
• Postmenopausal: atrophy, polyp, leiomyoma, endometrial hyperplasia/cancer, cervical dysplasia/cancer
History & exam
• Age, menopausal status, gestational age if preg.; volume & duration of current bleeding
• If premenopausal: menstrual hx including age of onset, interval between & duration of menses, any assoc. sx and LMP to assess timing of menstrual cycle
• Past Ob/Gyn hx (any structural abnl, STD and contraception)
• Health maint. (Pap smear, HPV screening); domestic violence; anticoag or antiplt meds
• General physical & abdominal exam (incl. tenderness, masses)
• Pelvic exam: external (quantity of bleeding seen on vulva, any lesions, any trauma); also, w/ assistance from Ob/Gyn, speculum exam (quantity of bleeding; cervical os open or close and if open, dilation; any polyps) & bimanual exam (uterine size and tenderness, adnexal mass and tenderness)
Laboratory evaluation & imaging
• Urine (rapid test) & serum pregnancy test (bhCG); Hct/hemoglobin
• Pelvic U/S: visualize intrauterine preg to r/o ectopic; if preg., intrauterine not seen, & bHCG > discrim. zone → concern for ectopic; if bHCG < discrim. zone → follow bHCG; nl placental position to r/o placenta previa and likely severe abruption
•
Ectopic pregnancy is life-threatening diagnosis
, ∴
must rule out if Pt pregnant
VAGINAL DISCHARGE
Fluid or mucus from vagina, cervix or uterus
Etiologies
• Infectious: bacterial vaginosis, candida vulvovaginitis, trichomoniasis • Noninfectious: physiologic (in preg. or non-preg.), rupture of membranes, foreign-body rxn
Initial evaluation
• Age, LMP, gestational age if preg. or menopausal status
• Discharge quantity, color, consistency, odor, assoc. sx (itchiness, redness, abd/pelvic pain) • Past gyn hx incl STD and contraception usage (condoms ↓ STD risk) • Tampon or condom use as risk factors for retained foreign body • Pelvic exam: external (quantity & quality of discharge on vulva, any lesions); speculum (discharge, appearance of cervix), bimanual (cervical motion tenderness) • Laboratory: pH of discharge; microscopy (saline & KOH wet mounts); urine pregnancy test
Treatment
• Bacterial vaginosis: oral or vaginal metronidazole or clindamycin • Candida vulvovaginitis: oral or topical antimycotic medications • Trichomoniasis: oral metronidazole
ADNEXAL MASS IN NON-PREGNANT WOMAN
Mass arising from ovary, fallopian tube or surrounding connective tissue
Etiologies
• Ovarian: functional (follicular and corpus luteum) or hemorrhagic cyst, endometriomas, ovarian torsion, tubo-ovarian abscess, benign & malignant ovarian tumors • Fallopian tube: paratubal cyst, hydrosalpinx, ovarian torsion, tubo-ovarian abscess
Initial evaluation
• LMP
menopausal status; associated sx of abd
pelvic pain, FHx of gyn cancers • Abd exam (distension, tenderness, masses); bimanual (uterine or adnexal masses)
• Preg. test if premenopausal (if, then mass likely pregnancy); CA-125 if postmenopausal • Pelvic U/S (even if mass first identified on CT as U/S is best modality); U/S appearance of mass most important factor used to determine risk of malignancy