Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (51 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

HEPATIC VASCULAR DISEASE
Portal vein thrombosis
(PVT) (
Al Phar Ther
2009;30:881;
J Hepatol
2012;56:S1)
• Definition: thrombosis, constriction or invasion of portal vein → portal HTN → varices. Isolated splenic vein thrombosis (eg, 2° to pancreatitis) → isolated gastric varices.
• Etiologies: cirrhosis, neoplasm (pancreas, HCC), abdominal infxn → pylephlebitis (infected thrombosis of PVT), hypercoag state (incl MPS), pancreatitis, IBD, surgery, trauma • Clinical manifestations
acute PVT
: can p/w pain; often asx and dx as incidental finding on U/S or CT if mesenteric vein involved may p/w intestinal infarct; if fever consider pylephlebitis
chronic PVT
: asx/incidental finding; may p/w s/s of portal HTN → hematemesis 2° variceal bleeding, splenomegaly, mild enceph; ascites uncommon unless cirrhosis
• Diagnostic studies: LFTs usually normal; U/S w/ Doppler, MRA, CT (I
+
), angiography;
“portal cavernoma” network of hepatopedal collaterals in chronic PVT—can rarely cause biliary obstruction and cholestatic LFTs = portal cholangiopathy (may require surgery)
• Treatment: eval for underlying cause (cirrhosis, MDS, hypercoag); if cirrhotic, Rx less clear
acute
: LMWH → warfarin × 6 mo, or indefinitely if irreversible cause (except cirrhosis),
chronic
: anticoag if noncirrhotic or hypercoag state; unclear if benefit > bleed risk
ppx
: LMWH may prevent PVT & liver decomp in advanced cirrhosis (
Gastro
2012;143:1253)
Varices: screen at dx; no evidence for 1° ppx of bleed; if bleed endoscopic Rx and bB. If refractory bleed consider TIPS, shunt. Isolated gastric varices 2° splenic vein thrombosis: splenectomy is curative.
Budd-Chiari syndrome
(
J Hepatol
2012;56:S1)
• Occlusion of hepatic vein(s) or IVC → sinusoidal congestion and portal HTN
• Etiol: ~50% due to myeloproliferative disorder a/w
JAK2
mutations (esp.
P. vera
), other hypercoag state, tumor invasion (HCC, renal, adrenal), IVC webs, trauma,
1
/
4
idiopathic • Symptoms: hepatomegaly, RUQ pain, ascites, dilated venous collaterals • Dx: ± ↑ aminotransferases & AΦ; Doppler U/S of hepatic veins (85% Se & Sp); CT (I
+
) or MRI/MRV → vein occlusion or ↑ caudate lobe (separate venous drainage); “spider-web” pattern on hepatic venography; liver bx showing congestion (r/o right-sided CHF) • Treatment: anticoag (LMWH → warfarin); consider thrombolysis acutely; if short stenosis stent may be possible; consider TIPS (↑ occlusion risk c/w side-to-side portocaval shunt); liver transplant if hepatic failure or failed shunt (
J Gastro Surg
2012;16:286)
Sinusoidal obstruction syndrome
(SOS) (
J Hepatol
2012;56:S1)
•
Occlusion of hepatic venules and sinusoids (formerly veno-occlusive disease
) • Etiologies: HSCT, chemo (esp. cyclopho), XRT, Jamaican bush tea • Clinical manifestations: hepatomegaly, RUQ pain, ascites, weight gain, ↑ bilirubin • Dx: U/S w/ reversal of portal flow, but often not helpful; dx made clinically (↑ bili, wt gain/ascites and RUQ pain) or, if necessary, by liver bx or HVPG (>10 mmHg) • Treatment (20% mortality): supportive; ? defibrotide (adenosine agonist ↑ TPA levels) • Ppx: defibrotide; ursodeoxycholic acid for high-risk HSCT pop; ? use of low-dose heparin
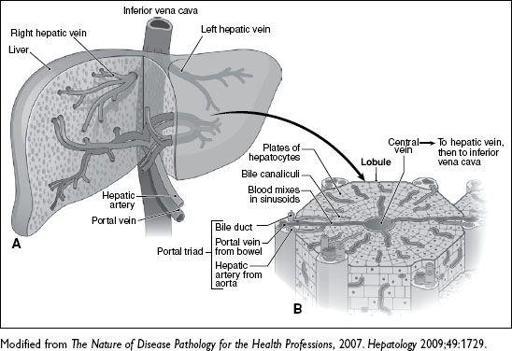
Figure 3-8
Hepatic vasculature
ASCITES
Pathophysiology
• Portal hypertension → systemic vasodilatation (? due to release of NO) → ↓ effective arterial volume → renal Na retention • ↓ serum oncotic pressure from hypoalbuminemia; ↑ hepatic lymph production
Symptoms
• ↑ abd girth, wt gain, new abd hernia, abd pain, dyspnea, nausea, early satiety
Evaluation
(
JAMA
2008;299:1166;
Hepatology
2009;29:2087)
• Physical exam: flank dullness (NPV
90%; >1500 mL needed), shifting dullness (Se
83%) •
Radiologic: U/S
detects >100 mL; MRI/CT (also help with Ddx) •
Paracentesis
(
NEJM
2006
;
355:e21;
Dig Dis Sci
2007;52:3307): perform in all Pts w/ new ascites and consider in all hospitalized cirrhotics w/ ascites; complic. <1% (bleeding, but risk not related to PT or plt count;
Hepatology
2004;40:484); U/S ↑ success but does not ↓ complic.
•
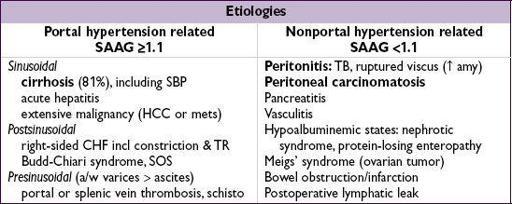
Serum-ascites albumin gradient (SAAG)
: ~95% acc. for portal HTN (
Annals
1992;117:215)
≥1.1 g/dL → portal hypertension related; <1.1 g/dL → non–portal hypertension related
if portal HTN + another cause (seen in ~5% of cases) SAAG still ≥1.1
if known cirrhosis and SAAG <1.1 but no other readily identifiable cause, likely just cirrhosis (
Am J Gastro
2009;104:1401)
• Ascites fluid total protein (AFTP): useful when SAAG ≥1.1 to distinguish cirrhosis (AFTP <2.5 g/dL) from cardiac ascites (AFTP ≥ 2.5 g/dL) •
Rule out infection
: cell count w/ diff + Gram stain/cx define bacterial peritonitis (see later); bedside inoculation of cx bottles ↑ yield to 90% (
Gastro
1988;95:1351) fungal cx if prolonged hosp, abx use; AFB cx + adenosine deaminase to r/o TB
• Other tests: amylase (pancreatitis, gut perforation); triglycerides (chylous ascites); cytology (peritoneal carcinomatosis, ~95% Se w/ 3 samples); LDH, glc, CEA, AΦ (perforation)
Treatment
•
If 2° to portal HTN (see “Cirrhosis” for details): ↓ Na intake
+
diuretics
(spironolactone + furosemide); if refractory → large-volume paracentesis or TIPS
• If non–portal HTN related: depends on underlying cause (TB, malignancy, etc.) • Vaptans ↑ Na, mobilize ascites, but no morb/mort benefit (
Al Pharm & Ther
2012;36:619)
Bacterial peritonitis
(
Gut
2012;61:297)
•
SBP/CNNA
: seen in cirrhosis (qv) b/c ascites have ↓ opsonins; rare in other causes •
NNBA
: often resolves w/o Rx; follow closely → Rx only if sx or persistently culture
•
Secondary
intra-abdominal abscess or perforation so often polymicrobial ascitic fluid TP >1 g/dL, glc <50 mg/dL, LDH >225 U, CEA >5, AΦ >240 Rx: 3rd-gen. ceph + metronidazole; urgent abdominal imaging ± ex lap •
Peritoneal dialysis-associated
: cloudy fluid, abd pain, fever, nausea pathogens: 70% GPC, 30% GNR; Rx: vanc + gent (IV load, then administer in PD)
BILIARY TRACT DISEASE
CHOLELITHIASIS (GALLSTONES)
Epidemiology & pathogenesis
(
J Hep
2008;48:S124)
• >10% adults in the U.S. have gallstones; a/w ↑ overall mortality (
Gastro
2011;140:508) • Bile = bile salts, phospholipids, cholesterol; ↑ cholesterol saturation in bile + accelerated nucleation + gallbladder hypomotility → gallstones • Risk factors: ; South, Central, Native American; ↑ age (>40 y), obesity, pregnancy, TPN, rapid ↓ wt; drugs (OCPs, estrogen, clofibrate, octreotide, ceftriaxone); ileal disease • ? statin use >1 y ↓ risk of sx gallstones & cholecystectomy (
; South, Central, Native American; ↑ age (>40 y), obesity, pregnancy, TPN, rapid ↓ wt; drugs (OCPs, estrogen, clofibrate, octreotide, ceftriaxone); ileal disease • ? statin use >1 y ↓ risk of sx gallstones & cholecystectomy (
JAMA
2009;302:2001)
Types of gallstones
• Cholesterol (90%): 2 subtypes
mixed: contain >50% cholesterol; typically smaller, multiple stones
pure: 100% cholesterol; larger, yellow, white appearance
• Pigment (10%)
Black:
unconjugated bilirubin (chronic hemolysis, cirrhosis) and calcium
Brown:
stasis & infection in bile ducts → bacteria deconjugate bilirubin → precipitates w/ calcium; seen w/ duodenal diverticula, biliary strictures, parasites