Ross & Wilson Anatomy and Physiology in Health and Illness (159 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

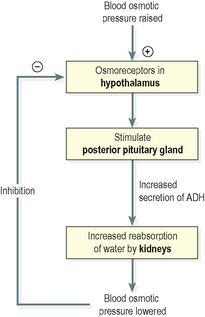
Figure 13.13
Negative feedback regulation of secretion of antidiuretic hormone (ADH).
Aldosterone
Secreted by the adrenal cortex, this hormone increases the reabsorption of sodium and water, and the excretion of potassium. Secretion is regulated through a negative feedback system (
Fig. 13.14
).
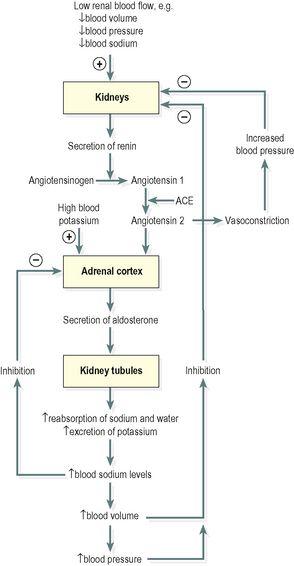
Figure 13.14
Negative feedback regulation of aldosterone secretion.
ACE = angiotensin converting enzyme.
Atrial natriuretic peptide
Also known as ANP, this hormone is secreted by the atria of the heart in response to stretching of the atrial wall. It decreases reabsorption of sodium and water from the proximal convoluted tubules and collecting ducts. Secretion of ANP is also regulated by a negative feedback system (
Fig. 13.15
).
Figure 13.15
Negative feedback regulation of secretion of atrial natriuretic peptide (ANP).
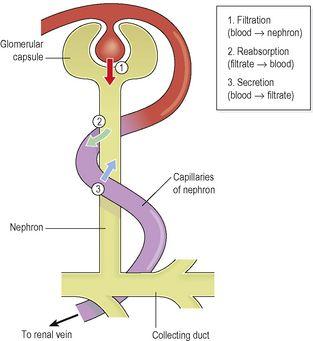
Tubular secretion (
Fig. 13.12
)
Filtration occurs as the blood flows through the glomerulus. Substances not required and foreign materials, e.g. drugs including penicillin and aspirin, may not be cleared from the blood by filtration because of the short time it remains in the glomerulus. Such substances are cleared by secretion from the peritubular capillaries into the convoluted tubules and excreted from the body in the urine. Tubular secretion of hydrogen ions (H
+
) is important in maintaining normal blood pH.
Summary of urine formation
The three processes involved – filtration, selective reabsorption and tubular secretion – are described above and summarised in
Figure 13.16
.
Figure 13.16
Summary of the three processes that form urine.
Composition of urine
Water 96%
Urea 2%
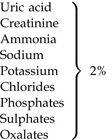
Urine is clear and amber in colour due to the presence of urobilin, a bile pigment altered in the intestine, reabsorbed then excreted by the kidneys (see
Fig. 12.37, p. 303
). The specific gravity is between 1020 and 1030, and the pH is around 6 (normal range of 4.5 to 8). A healthy adult passes 1000 to 1500 ml per day. The amount of urine produced and the specific gravity vary according to fluid intake and the amount of solute excreted. Urine production is decreased during sleep and exercise.
Water balance and urine output
The source of most body water is dietary food and fluid, and a small amount (called ‘metabolic water’) is formed by metabolic processes. Water is excreted as the main constituent of urine, in expired air, faeces and through the skin as sweat. The amount lost in expired air and faeces is fairly constant, and the amount of sweat produced is associated with environmental and body temperatures (
p. 358
).
The balance between fluid intake and output is controlled by the kidneys. The minimum urinary output, i.e. the smallest volume required to excrete body waste products, is about 500 ml per day. Urinary volume in excess of this is controlled mainly by antidiuretic hormone (ADH) released into the blood by the posterior lobe of the pituitary gland. The posterior pituitary is closely related to the hypothalamus in the brain (see
Fig. 9.3A and B, p. 210
).
Sensory nerve cells in the hypothalamus (osmoreceptors) detect changes in the osmotic pressure of the blood. Nerve impulses from the osmoreceptors stimulate the posterior pituitary to release ADH. When the osmotic pressure is raised, i.e. the blood is becoming more concentrated, ADH output is increased and as a result, water reabsorption by the distal convoluted tubules and collecting ducts is increased, reducing the blood osmotic pressure and ADH output. This negative feedback mechanism maintains the blood osmotic pressure (and therefore sodium and water concentrations) within normal limits (see
Fig. 13.13
).
The feedback mechanism may be suppressed when there is an excessive amount of a dissolved substance in the blood. For example, in diabetes mellitus when the blood glucose level is above the transport maximum of the renal tubules, excess water is excreted with the excess glucose. This
polyuria
may lead to dehydration despite increased production of ADH but is usually accompanied by acute thirst and increased water intake.
When blood volume is increased, stretch receptors in the atria of the heart release atrial natriuretic hormone (ANP). This reduces reabsorption of sodium and water by the proximal convoluted tubules and collecting ducts, meaning that more sodium and water are excreted. In turn, this lowers blood volume and reduces atrial stretching, and through the negative feedback mechanism ANP secretion is switched off (see
Fig. 13.15
). Raised ANP levels also inhibit secretion of ADH and aldosterone, further promoting loss of sodium and water.
Electrolyte balance
Changes in the concentration of electrolytes in the body fluids may be due to changes in:
•
the body water content, or
•
electrolyte levels.
There are several mechanisms that maintain the balance between water and electrolyte concentration.
Sodium and potassium balance
Sodium is the most common cation (positively charged ion) in extracellular fluid and potassium is the most common intracellular cation.
Sodium is a constituent of almost all foods and salt is often added to food during cooking. This means that intake is usually in excess of the body’s needs. It is excreted mainly in urine and sweat.
The amount of sodium excreted in sweat is insignificant except when sweating is excessive. This may occur when there is pyrexia (fever), a high environmental temperature or during sustained physical exercise. Normally the renal mechanism described below maintains the concentration of sodium and potassium within physiological limits. When excessive sweating is sustained, e.g. living in a hot climate or working in a hot environment, acclimatisation occurs in about 7 to 10 days and the amount of electrolytes lost in sweat is reduced.
Sodium and potassium occur in high concentrations in digestive juices – sodium in gastric juice and potassium in pancreatic and intestinal juice. Normally these ions are reabsorbed by the colon, but following acute and prolonged diarrhoea they may be excreted in large quantities with resultant electrolyte imbalance.
Renin–angiotensin–aldosterone system (
Fig. 13.14
)
Sodium is a normal constituent of urine and the amount excreted is regulated by the hormone
aldosterone
, secreted by the adrenal cortex. Cells in the afferent arteriole of the nephron release the enzyme
renin
in response to sympathetic stimulation, low blood volume or by low arterial blood pressure. Renin converts the plasma protein
angiotensinogen
, produced by the liver, to angiotensin 1.
Angiotensin converting enzyme
(ACE), formed in small quantities in the lungs, proximal convoluted tubules and other tissues, converts angiotensin 1 into angiotensin 2, which is a very potent vasoconstrictor and increases blood pressure. Renin and raised blood potassium levels also stimulate the adrenal gland to secrete aldosterone. Water is reabsorbed with sodium and together they increase the blood volume, leading to reduced renin secretion through the negative feedback mechanism. When sodium reabsorption is increased potassium excretion is increased, indirectly reducing intracellular potassium.
As described above, ANP is also involved in the regulation of sodium levels.
Calcium balance
Regulation of calcium levels is achieved by coordinated secretion of parathyroid hormone (PTH,
p. 215
) and calcitonin (
p. 214
). The distal collecting tubules reabsorb more calcium in response to PTH secretion, and reabsorb less calcium in response to secretion of calcitonin.