Ross & Wilson Anatomy and Physiology in Health and Illness (78 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

•
The bladder
wall relaxes.
•
The metabolic rate
is greatly increased.
Parasympathetic stimulation
•
The liver
. The secretion of bile is increased.
•
The stomach
and
small intestine
. Motility and secretion are increased, together with the rate of digestion and absorption of food.
•
The pancreas
. The secretion of pancreatic juice is increased.
•
Urethral
and
anal sphincters
. Relaxation of the internal urethral sphincter is accompanied by contraction of the muscle of the bladder wall, and micturition occurs. Similar relaxation of the internal anal sphincter is accompanied by contraction of the muscle of the rectum, and defecation occurs. In both cases there is voluntary relaxation of the external sphincters.
•
The adrenal glands
. No effect.
•
The metabolic rate
. No effect.
Eye
Sympathetic stimulation
This causes contraction of the radiating muscle fibres of the iris, dilating the pupil. Retraction of the levator palpebrae muscles occurs, opening the eyes wide and giving the appearance of alertness and excitement. The ciliary muscle that adjusts the thickness of the lens is slightly relaxed, facilitating distant vision.
Parasympathetic stimulation
This contracts the circular muscle fibres of the iris, constricting the pupil. The eyelids tend to close, giving the appearance of sleepiness. The ciliary muscle contracts, facilitating near vision.
Skin
Sympathetic stimulation
•
Increases sweat secretion, leading to increased heat loss from the body.
•
Contracts the arrector pili (the muscles in the hair follicles of the skin), giving the appearance of ‘goose flesh’.
•
Constricts the peripheral blood vessels, increasing blood supply available to active organs, e.g. the heart and skeletal muscle.
There is no parasympathetic nerve supply to the skin. Some sympathetic fibres are adrenergic, causing vasoconstriction, and some are cholinergic, causing vasodilation (see
Fig. 7.8
,
p. 143
).
Afferent impulses from viscera
Sensory fibres from the viscera travel with autonomic fibres and are sometimes called
autonomic afferents
. The impulses they transmit are associated with:
•
visceral reflexes, usually at an unconscious level, e.g. cough, blood pressure (baroreceptors)
•
sensation of, e.g., hunger, thirst, nausea, sexual sensation, rectal and bladder distension
•
visceral pain.
Visceral pain
Normally the viscera are insensitive to cutting, burning and crushing. However, a sensation of dull, poorly located pain is experienced when:
•
visceral nerves are stretched
•
a large number of fibres are stimulated
•
there is ischaemia and local accumulation of metabolites
•
the sensitivity of nerve endings to painful stimuli is increased, e.g. during inflammation.
If the cause of the pain, e.g. inflammation, affects the parietal layer of a serous membrane (pleura, peritoneum) the pain is acute and easily located over the site of inflammation. This is because the peripheral spinal (somatic) nerves that innervate the superficial tissues also innervate the parietal layer of serous membrane. They transmit the impulses to the cerebral cortex where somatic pain is perceived and accurately located. Appendicitis is an example of this type of pain. Initially it is dull and vaguely located around the midline of the abdomen. As the condition progresses the parietal peritoneum becomes involved and acute pain is clearly located in the right iliac fossa, i.e. over the appendix.
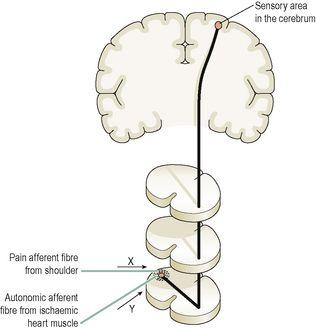
Referred pain (
Fig. 7.48
)
In some cases of visceral disease, pain may be perceived to occur in superficial tissues remote from its site of origin, i.e. referred pain. This occurs when sensory fibres from the affected organ enter the same segment of the spinal cord as somatic nerves, i.e. those from the superficial tissues. It is believed that the sensory nerve from the damaged organ stimulates the closely associated nerve in the spinal cord and it transmits the impulses to the sensory area in the cerebral cortex where the pain is perceived as originating in the area supplied by the somatic nerve. Examples of referred pain are given in
Table 7.3
.
Figure 7.48
Referred pain.
Ischaemic heart tissue generates impulses in nerve Y that then stimulate nerve X and pain is perceived in the shoulder.
Table 7.3
Referred pain
| Tissue of origin of pain | Site of referred pain |
|---|---|
| Heart | Left shoulder |
 | Right shoulder |
 | Loin and groin |
| Uterus | Low back |
| Male genitalia | Low abdomen |
| Prolapsed intervertebral disc | Leg |
Disorders of the brain
Learning outcomes
After studying this section you should be able to:
list three causes of raised intracranial pressure (ICP)
relate the effects of raised ICP to the functions of the brain and changes in vital signs
outline how the brain is damaged during different types of head injury
describe four complications of head injury
explain the effects of cerebral hypoxia and stroke