Ross & Wilson Anatomy and Physiology in Health and Illness (157 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Figure 13.4
A longitudinal section of the right kidney.
The hilum
is the concave medial border of the kidney where the renal blood and lymph vessels, the ureter and nerves enter.
The renal pelvis
is the funnel-shaped structure that collects urine formed by the kidney (
Fig. 13.4
). Urine formed in the kidney passes through a renal
papilla
at the apex of a pyramid into a minor calyx, then into a major calyx before passing through the renal pelvis into the ureter. The walls of the pelvis contain smooth muscle and are lined with transitional epithelium. Peristalsis of the smooth muscle originating in pacemaker cells in the walls of the calyces propels urine through the renal pelvis and ureters to the bladder. This is an intrinsic property of the smooth muscle, and is not under nerve control.
Microscopic structure of the kidney
The kidney is composed of about 1–2 million functional units, the
nephrons
, and a smaller number of
collecting ducts
. The collecting ducts transport urine through the pyramids to the calyces and renal pelvis, giving the pyramids their striped appearance (
Fig. 13.4
). The collecting ducts are supported by a small amount of connective tissue, containing blood vessels, nerves and lymph vessels.
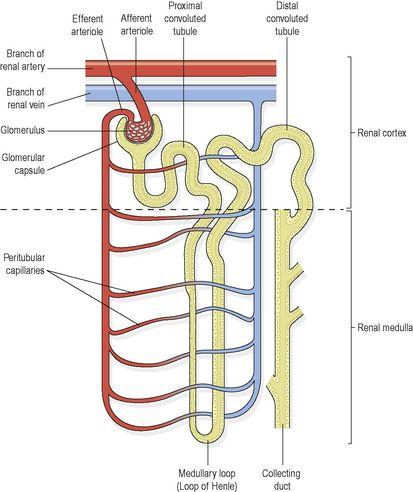
The nephron (
Fig. 13.5
)
The nephron consists of a tubule closed at one end, the other end opening into a collecting tubule. The closed or blind end is indented to form the cup-shaped
glomerular capsule
(Bowman’s capsule), which almost completely encloses a network of tiny arterial capillaries, the
glomerulus
. These resemble a coiled tuft and are shown in
Figure 13.6
. Continuing from the glomerular capsule, the remainder of the nephron is about 3 cm long and is described in three parts:
•
the proximal convoluted tubule
•
the medullary loop (loop of Henle)
•
the distal convoluted tubule, leading into a collecting duct.
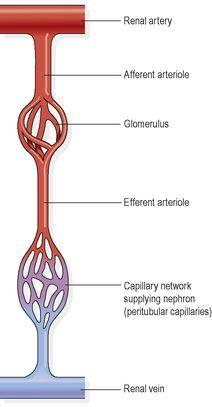
Figure 13.5
A nephron and associated blood vessels.
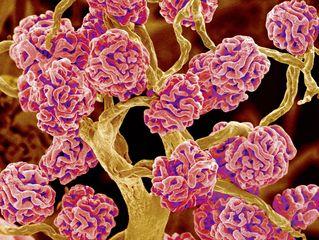
Figure 13.6
Coloured scanning electron micrograph of glomerular capillary tufts.
The collecting ducts unite, forming larger ducts that empty into the minor calyces.
The kidneys receive about 20% of the cardiac output. After entering the kidney at the hilum the renal artery divides into smaller arteries and arterioles. In the cortex an arteriole, the
afferent arteriole
, enters each glomerular capsule and then subdivides into a cluster of tiny arterial capillaries, forming the glomerulus. Between these capillary loops are connective tissue phagocytic
mesangial cells
, which are part of the monocyte–macrophage system (
p. 36
). The blood vessel leading away from the glomerulus is the
efferent arteriole
. The afferent arteriole has a larger diameter than the efferent arteriole, which increases pressure inside the glomerulus and drives filtration across the glomerular capillary walls (
Fig. 13.7
). The efferent arteriole divides into a second peritubular (meaning ‘around tubules’) capillary network, which wraps around the remainder of the tubule, allowing exchange between the fluid in the tubule and the bloodstream (
Figs 13.5
,
13.8
and
13.10
). This maintains the supply of oxygen and nutrients to the local tissues and removes waste products. Venous blood drained from this capillary bed eventually leaves the kidney in the renal vein, which empties into the inferior vena cava.
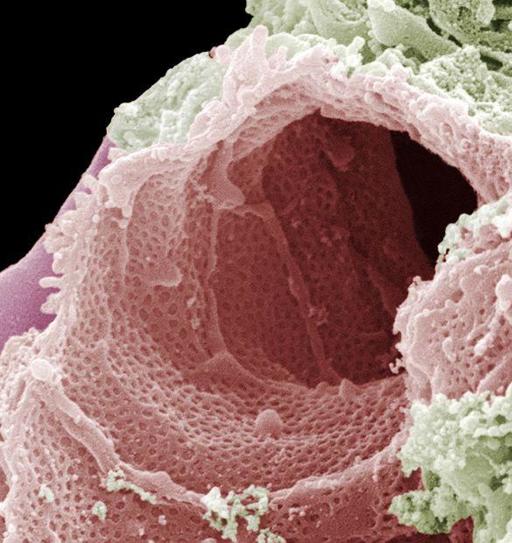
Figure 13.7
Coloured scanning electron micrograph of glomerular capillary.
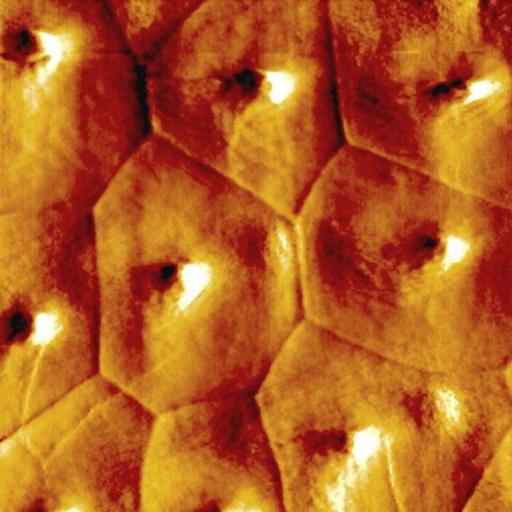
Figure 13.9
Simple squamous epithelium of the collecting ducts. Coloured atomic force micrograph.
The walls of the glomerulus and the glomerular capsule consist of a single layer of flattened epithelial cells. The glomerular walls are more permeable than those of other capillaries. The remainder of the nephron and the collecting duct are formed by a single layer of simple squamous epithelium (
Fig. 13.9
).
Figure 13.8
The series of blood vessels in the kidney.
The blood vessels of the kidney are supplied by both sympathetic and parasympathetic nerves. The presence of both branches of the autonomic nervous system controls renal blood vessel diameter and renal blood flow independently of autoregulation (
p. 334
).
Functions of the kidney
Formation of urine
The kidneys form urine, which passes through the ureters to the bladder for storage prior to excretion. The composition of urine reflects exchange of substances between the nephron and the blood in the renal capillaries. Waste products of protein metabolism are excreted, electrolyte levels are controlled and pH (acid–base balance) is maintained by excretion of hydrogen ions. There are three processes involved in the formation of urine:
•
filtration
•
selective reabsorption
•
secretion.
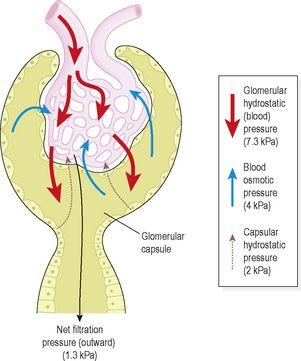
Filtration (
Fig. 13.11
)
This takes place through the semipermeable walls of the glomerulus (
Fig. 13.10
) and glomerular capsule. Water and other small molecules pass through, although some are reabsorbed later. Blood cells, plasma proteins and other large molecules are too large to filter through and therefore remain in the capillaries (see
Box 13.1
). The filtrate in the glomerulus is very similar in composition to plasma with the important exceptions of plasma proteins and blood cells.