Ross & Wilson Anatomy and Physiology in Health and Illness (138 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

The
jejunum
is the middle section of the small intestine and is about 2 metres long.
The
ileum
, or terminal section, is about 3 metres long and ends at the
ileocaecal valve
, which controls the flow of material from the ileum to the
caecum
, the first part of the large intestine, and prevents regurgitation.
Structure of the small intestine
The walls of the small intestine are composed of the four layers of tissue shown in
Figure 12.2
. Some modifications of the peritoneum and mucosa (mucous membrane lining) are described below.
Peritoneum
A double layer of peritoneum called the
mesentery
attaches the jejunum and ileum to the posterior abdominal wall (see
Fig. 12.3A
). The attachment is quite short in comparison with the length of the small intestine, therefore it is fan shaped. The large blood vessels and nerves lie on the posterior abdominal wall and the branches to the small intestine pass between the two layers of the mesentery.
Mucosa
The surface area of the small intestine mucosa is greatly increased by permanent circular folds, villi and microvilli.
The
permanent circular folds
, unlike the rugae of the stomach, are not smoothed out when the small intestine is distended (
Fig. 12.25
). They promote mixing of chyme as it passes along.
Figure 12.25
Section of a small piece of small intestine (opened out), showing the permanent circular folds.
The
villi
are tiny finger-like projections of the mucosal layer into the intestinal lumen, about 0.5 to 1 mm long (
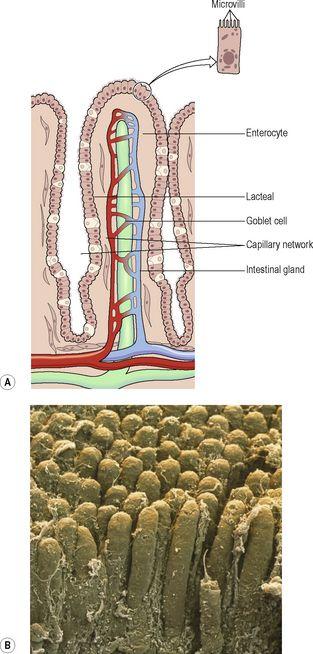
Fig. 12.26
). Their walls consist of columnar epithelial cells, or
enterocytes
, with tiny
microvilli
(1 μm long) on their free border.
Goblet cells
(see also
Fig. 12.5
) that secrete mucus are interspersed between the enterocytes. These epithelial cells enclose a network of blood and lymph capillaries. The lymph capillaries are called
lacteals
because absorbed fat gives the lymph a milky appearance. Absorption and some final stages of digestion of nutrients take place in the enterocytes before entering the blood and lymph capillaries.
Figure 12.26
A.
A highly magnified diagram of one complete villus in the small intestine.
B.
Coloured scanning electron micrograph showing many villi.
The
intestinal glands
are simple tubular glands situated below the surface between the villi. The cells of the glands migrate upwards to form the walls of the villi replacing those at the tips as they are rubbed off by the intestinal contents. The entire epithelium is replaced every 3 to 5 days. During migration, the cells form digestive enzymes that lodge in the microvilli and, together with intestinal juice, complete the chemical digestion of carbohydrates, protein and fats.
Numerous
lymph nodes
are found in the mucosa at irregular intervals throughout the length of the small intestine. The smaller ones are known as
solitary lymphatic follicles
, and about 20 or 30 larger nodes situated towards the distal end of the ileum are called
aggregated lymphatic follicles
(Peyer’s patches,
Fig. 12.25
). These lymphatic tissues, packed with defensive cells, are strategically placed to neutralise ingested antigens (
Ch. 15
).
Blood supply
The
superior mesenteric artery
supplies the whole of the small intestine, and venous drainage is by the
superior mesenteric vein
that joins other veins to form the portal vein (see
Figs 5.45
and
5.46
,
pp. 102 and 103
). The portal vein contains a high concentration of absorbed nutrients and this blood passes through the liver before entering the hepatic veins and, ultimately, into the inferior vena cava (see
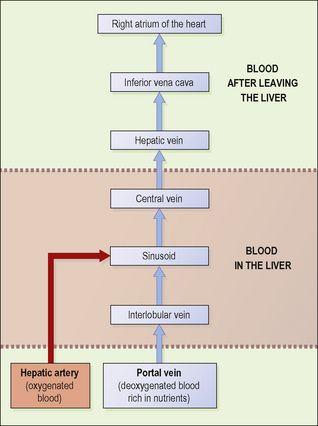
Fig. 12.36
).
Figure 12.36
Scheme of blood flow through the liver.
Intestinal juice
About 1500 ml of intestinal juice are secreted daily by the glands of the small intestine. It consists of:
•
water
•
mucus
•
mineral salts.
The pH of intestinal juice is usually between 7.8 and 8.0.
Functions of the small intestine
The functions are:
•
onward movement of its contents by peristalsis, which is increased by parasympathetic stimulation
•
secretion of intestinal juice, also increased by parasympathetic stimulation
•
completion of chemical digestion of carbohydrates, protein and fats in the enterocytes of the villi
•
protection against infection by microbes that have survived the antimicrobial action of the hydrochloric acid in the stomach, by the solitary lymph follicles and aggregated lymph follicles
•
secretion of the hormones cholecystokinin (CCK) and secretin
•
absorption of nutrients.
Chemical digestion in the small intestine
When acid chyme passes into the small intestine it is mixed with
pancreatic juice
,
bile
and
intestinal juice
, and is in contact with the enterocytes of the villi. In the small intestine digestion of all the nutrients is completed:
•
carbohydrates are broken down to monosaccharides
•
proteins are broken down to amino acids
•
fats are broken down to fatty acids and glycerol.
Pancreatic juice
Pancreatic juice is secreted by the exocrine pancreas (
p. 300
) and enters the duodenum at the duodenal papilla. It consists of:
•
water
•
mineral salts
•
enzymes:
–
amylase
–
lipase
–
nucleases that digest DNA and RNA
•
inactive enzyme precursors including:
–
trypsinogen
–
chymotrypsinogen.
Pancreatic juice is alkaline (pH 8) because it contains significant quantities of bicarbonate ions, which are alkaline in solution. When acid stomach contents enter the duodenum they are mixed with pancreatic juice and bile and the pH is raised to between 6 and 8. This is the pH at which the pancreatic enzymes, amylase and lipase, act most effectively.
Functions
Digestion of proteins
Trypsinogen and chymotrypsinogen are inactive enzyme precursors activated by
enterokinase
, an enzyme in the microvilli, which converts them into the active proteolytic enzymes
trypsin
and
chymotrypsin
. These enzymes convert polypeptides to tripeptides, dipeptides and amino acids. It is important that they are produced as inactive precursors and are activated only upon arrival in the duodenum, otherwise they would digest the pancreas.
Digestion of carbohydrates
Pancreatic amylase
converts all digestible polysaccharides (starches) not acted upon by salivary amylase to disaccharides.
Digestion of fats
Lipase
converts fats to fatty acids and glycerol. To aid the action of lipase,
bile salts
emulsify fats, i.e. reduce the size of the globules, increasing their surface area.
Control of secretion
The secretion of pancreatic juice is stimulated by secretin and CCK, produced by endocrine cells in the walls of the duodenum. The presence in the duodenum of acid chyme from the stomach stimulates the production of these hormones (see
Fig. 12.22
).
Bile
Bile, secreted by the liver, is unable to enter the duodenum when the hepatopancreatic sphincter is closed; therefore it passes from the
hepatic duct
along the
cystic duct
to the gall bladder where it is stored (see
Fig. 12.38
).
Bile has a pH of around 8 and between 500 and 1000 ml are secreted daily. It consists of:
•
water
•
mineral salts
•
mucus
•
bile salts
•
bile pigments, mainly bilirubin
•
cholesterol.
Functions
•
The bile salts emulsify fats in the small intestine.
•
Fatty acids are insoluble in water, which makes them very difficult to absorb through the intestinal wall. Bile salts make cholesterol and fatty acids soluble, enabling both these and fat-soluble vitamins (i.e. vitamins A, D, E and K) to be readily absorbed.
•
The bile pigment,
bilirubin
, is a waste product of the breakdown of erythrocytes and is excreted in the bile rather than in the urine because of its low solubility in water. Bilirubin is altered by microbes in the large intestine. Some of the resultant
urobilinogen
, which is highly water-soluble, is reabsorbed and then excreted in the urine, but most is converted to
stercobilin
and excreted in the faeces (see
Fig. 12.37
).
•
Stercobilin colours and deodorises the faeces.
Release from the gall bladder
After a meal, the duodenum secretes the hormones secretin and CCK during the intestinal phase of gastric secretion (
p. 292
). They stimulate contraction of the gall bladder and relaxation of the hepatopancreatic sphincter, enabling the bile and pancreatic juice to pass through the duodenal papilla into the duodenum together. Secretion is markedly increased when chyme entering the duodenum contains a high proportion of fat.