Ross & Wilson Anatomy and Physiology in Health and Illness (137 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Figure 12.22
The three phases of secretion of gastric juice.
1 Cephalic phase
This flow of juice occurs before food reaches the stomach and is due to reflex stimulation of the vagus (parasympathetic) nerves initiated by the sight, smell or taste of food. When the vagus nerves have been cut (vagotomy), this phase of gastric secretion stops. Sympathetic stimulation, e.g. during emotional states, also inhibits gastric activity.
2 Gastric phase
When stimulated by the presence of food the
enteroendocrine cells
in the pylorus (
Fig. 12.21
) and duodenum secrete
gastrin
, a hormone which passes directly into the circulating blood. Gastrin, circulating in the blood which supplies the stomach, stimulates the gastric glands to produce more gastric juice. In this way secretion of digestive juice is continued after completion of a meal and the end of the cephalic phase. Gastrin secretion is suppressed when the pH in the pylorus falls to about 1.5.
3 Intestinal phase
When the partially digested contents of the stomach reach the small intestine, two hormones,
secretin
and
cholecystokinin
, are produced by endocrine cells in the intestinal mucosa. They slow down the secretion of gastric juice and reduce gastric motility. By slowing the emptying rate of the stomach, the chyme in the duodenum becomes more thoroughly mixed with bile and pancreatic juice. This phase of gastric secretion is most marked following a meal with a high fat content.
The rate at which the stomach empties depends largely on the type of food eaten. A carbohydrate meal leaves the stomach in 2 to 3 hours, a protein meal remains longer and a fatty meal remains in the stomach longest.
Functions of the stomach
These include:
•
temporary storage allowing time for the digestive enzymes, pepsins, to act
•
chemical digestion – pepsins convert proteins to polypeptides
•
mechanical breakdown – the three smooth muscle layers enable the stomach to act as a churn, gastric juice is added and the contents are liquefied to chyme. Gastric motility and secretion are increased by parasympathetic nerve stimulation
•
limited absorption of water, alcohol and some lipid-soluble drugs
•
non-specific defence against microbes – provided by hydrochloric acid in gastric juice. Vomiting may occur in response to ingestion of gastric irritants, e.g. microbes or chemicals
•
preparation of iron for absorption further along the tract – the acid environment of the stomach solubilises iron salts, which is required before iron can be absorbed
•
production and secretion of intrinsic factor needed for absorption of vitamin B
12
in the terminal ileum
•
regulation of the passage of gastric contents into the duodenum. When the chyme is sufficiently acidified and liquefied, the pylorus forces small jets of gastric contents through the pyloric sphincter into the duodenum. The sphincter is normally closed, preventing backflow of chyme into the stomach
•
secretion of the hormone gastrin (see above).
Small intestine (
Figs 12.23
and
12.24
)
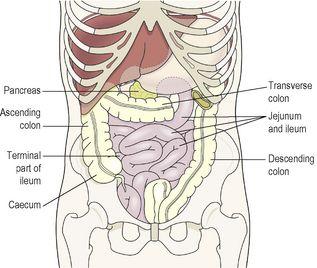
Figure 12.23
The duodenum and its associated structures.
Figure 12.24
The jejunum and ileum and their related structures.
Learning outcomes
After studying this section, you should be able to:
describe the location of the small intestine, with reference to surrounding structures
sketch a villus, labelling its component parts
discuss the digestive functions of the small intestine and its secretions
explain how nutrients are absorbed in the small intestine.
The small intestine is continuous with the stomach at the pyloric sphincter. The small intestine is a little over 5 metres long and leads into the large intestine at the
ileocaecal valve
. It lies in the abdominal cavity surrounded by the large intestine. In the small intestine the chemical digestion of food is completed and absorption of most nutrients takes place.
The small intestine comprises three continuous parts.
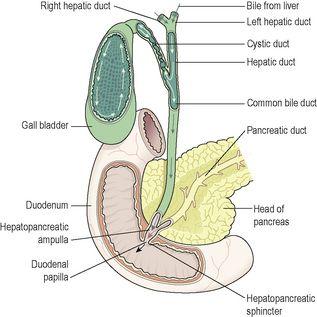
The
duodenum
is about 25 cm long and curves around the head of the pancreas. Secretions from the gall bladder and pancreas merge in a common structure – the
hepatopancreatic ampulla
– and enter the duodenum at the
duodenal papilla
. The duodenal papilla is guarded by a ring of smooth muscle, the
hepatopancreatic sphincter
(of Oddi) (see
Fig. 12.38
).
Figure 12.38
Direction of the flow of bile from the liver to the duodenum.