Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (86 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.39Mb size Format: txt, pdf, ePub
nb, Kernig’s or Brudzinski’s signsin only ~10% of Pts (
Lancet
2012;380:1684)
• ± Focal neuro findings (~30%; hemiparesis, aphasia, visual field cuts, CN palsies) • ± Funduscopic findings: papilledema, absent venous pulsations • ± Rash: maculopapular, petechial or purpuric
Diagnostic studies
(
Lancet
2012;380:1684)
•
Blood cultures ¥ 2
before abx
•
WBC count
: >10,000 in >90% of bacterial meningitis in healthy hosts •
Consider
head CT
to r/o mass effect before LP
if
presence of high-risk feature (age
>60 y, immunosupp., h/o CNS disease, new-onset seizure, Δ MS, focal neuro
findings, papilledema); absence of all these has NPV 97%; however, in Pts w/ mass effect, herniation may occur w/o LP and may not occur even w/ LP (
NEJM
2001;345:1727)
•
Lumbar puncture
(
NEJM
2006;355:e12)
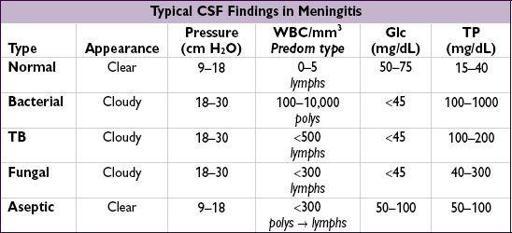
CSF Gram stain
has 30–90% Se; cx 80–90% Se if LP done prior to abx role of CSF PCR for common bacterial causes (? ~90% Se if w/in 2 h) to be defined repeat LP only if no clinical response after 48 h of appropriate abx or CSF shunt
Opening pressure
typically ↑ in bact meningitis; must measure w/ Pt’s legs extended
Rule of 2s
: CSF WBC >2k, glc <20, & TP >200 has >98% Sp for bacterial meningitis
Recurrent meningitis
• Bacterial: consider CSF leak, dermal sinus or other congenital/acquired anatomic defects • Viral: HSV-2 (causes majority of Mollaret’s meningitis) • Aseptic (see below): leak from cyst/tumor/lesion with dermoid/epidermoid elements, autoimmune (eg, SLE, Behçet’s), medications
• Additional CSF studies based on clinical suspicion: AFB smear & cx, India ink prep, cryptococcal Ag, fungal cx, VDRL, PCR (eg, of HSV, VZV, enteroviral), cytology
Prognosis
• For community-acquired
S. pneumo
mort. 19–37%; 30% have long-term neuro sequelae
ASEPTIC MENINGITIS
Definition
•
Negative bacterial micro data
, CSF pleocytosis withappropriate blood & CSF cultures (aseptic meningitis can be neutrophilic, though less common) • Aseptic = less likely to be bacterial, but can be infectious or noninfectious
Etiologies
(
Neurology
2006;66:75)
•
Viral
: enteroviruses (most common), HIV, HSV (type 2 > 1), VZV, mumps, lymphocytic choriomeningitis virus, encephalitis viruses, adenovirus, polio, CMV, EBV
•
Parameningeal focus of infection
(eg, brain abscess, epidural abscess, septic thrombophlebitis of dural venous sinuses or subdural empyema) •
Partially treated bacterial meningitis
•
TB
,
fungal
,
spirochetal
(Lyme, syphilis, leptospirosis),
rickettsial
,
Coxiella
,
Ehrlichia
•
Medications
: TMP/SMX, NSAIDs, IV Ig and antilymphocyte Ig, PCN, INH, lamotrigine •
Systemic illness
: SLE, sarcoidosis, Behçet’s, Sjögren’s syndrome, RA •
Neoplasm
: intracranial tumors (or cysts), lymphomatous or carcinomatous meningitis (CSF cytology or flow may be reactive and dx may require meningeal bx)
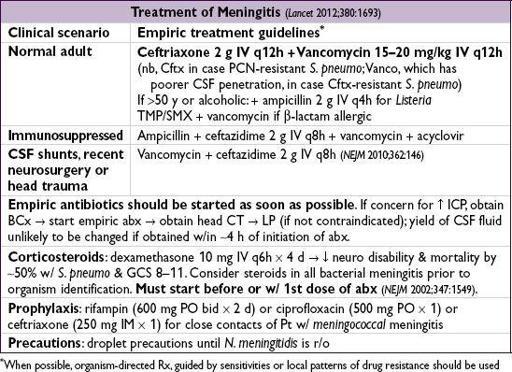
Empiric treatment
• No abx if suspect viral (cell count <500 w/ >50% lymphs, TP <80–100 mg/dL, normal glc,Gram stain, not elderly/immunosupp.); o/w start empiric abx, wait for cx data • If suspect MTb: antimycobacterial Rx + dexamethasone (
NEJM
2004;351:1741) • If suspect fungal: ampho lipid formulation, ± 5-fluorouracil
ENCEPHALITIS
Definition
• Infection of brain parenchyma with evidence of neurologic dysfunction
Etiologies
(specific etiology found in
<20% of cases;
Neurology
2006;66:75;
CID
2008;47:303)
•
HSV-1
(~9%): all ages/seasons; MRI: temporal lobe lesions/edema; EEG: temporal focus •
VZV
(~9%): 1° or reactivation; ± vesicular rash; all ages (favors elderly), all seasons •
Arboviruses
(~9%): Eastern/Western equine, St. Louis, Japanese, Powassan, W. Nile (
NEJM
2005;353:287): mosquito vector, bird reservoir; fever, HA,
flaccid paralysis
, rash. Risk factors for severe dis: renal dis., cancer, EtOH, DM, HTN (
Am J Trop Med Hyg
2012;87:179).
•
Enteroviruses
(coxsackie, echo): viral syndrome; peaks in late summer/early fall • Others: CMV, EBV, HIV, JC virus (PML), measles, mumps, rubella, rabies, flu, adenovirus • Nonviral mimics: bacterial endocarditis, brain abscess, toxoplasmosis, TB, toxins, vas-culitis, hematologic malignancies, Whipple’s disease, subdural hematoma, encephalomyelitis (eg, ADEM), paraneoplastic syndromes, seizure, mitochondrial disorders, autoimmune anti
N
-methyl-D-aspartate receptor (esp. if <30 y,
CID
2012;54:899)
Clinical manifestations
•
Fever
,
HA
, Δ MS, ± seizures and focal neuro findings (latter atypical for viral
meningitis
)
Diagnostic studies
(etiologic dx made in only about 25% of cases)
• Vaccine hx, dilated retinal exam, ELISA or DFA nasal/resp swabs for viruses, serologies •
Lumbar puncture
: lymphocytic pleocytosis; PCR for HSV (95% Se & Sp at 2–3 d), VZV, CMV, EBV, HIV, JC, adeno/enterovirus, W. Nile (<60% Se); W. Nile CSF IgM 80% Se •
MRI
(CT if MRI unavailable); W. Nile w/ thalamic hyperintensity • EEG to r/o seizure; findings in encephalitis are nonspecific
Treatment
• HSV, VZV: acyclovir 10 mg/kg IV q8h (often empiric Rx given frequency of HSV/VZV) • CMV: ganciclovir ± foscarnet; supportive care for most other etiologies
BELL’S PALSY
Definition & etiology
• Acute idiopathic unilat.
facial nerve palsy
(CN VII), often presumed HSV-1 reactivation
Clinical manifestations
• Unilateral
facial muscle weakness
,
hyperacusis
, ↓ taste/lacrimation/salivation
Diagnosis
• Dx of exclusion: r/o brainstem lesion, Lyme, zoster (incl
sine herpete
), HIV/AIDS, sarcoid
Treatment
(
NEJM
2007;357:1598;
JAMA
2009;302:985)
• ~80% recover spontaneously by 9 mo (much lower rate in DM) • Corticosteroids (prednisolone 25 mg PO bid × 10 d) started w/in 72 h of sx onset improve odds of recovery (note: no conclusive data for use in DM, immunosupp.) • No conclusive data to support the use of acyclovir or valacyclovir, though often prescribed
ZOSTER
Definition & etiology
• Zoster = herpes zoster = shingles: acute, unilat.,
painful dermatomal skin eruption
• VZV reactivation in peripheral nerve distribution from latency in dorsal root ganglion
Clinical manifestations
•
Neuritic pain in a dermatomal distribution
, then acute
dermatomal eruption of clustered rash
(vesicles > papules/pustules > macules) in varying stages of evolution • Consecutive dermatomes may be seen in all Pts; more widespread in immunosupp.
• Lesions in V1 distribution of facial nerve require urgent ophthalmologic evaluation • Post-herpetic neuralgia (PHN) = severe pain lasting >90 d after episode; may last mos to y, more frequent w/ ↑ age and delay of antiviral Rx
Diagnosis
• Appearance of rash; DFA is most Se from scrape of newly unroofed vesicle. Tzanck does not distinguish HSV or VZV, cx insensitive for VZV (unlike HSV).
Other books
The Confession by Charles Todd
My One and Only (Ardent Springs Book 3) by Terri Osburn
His One Desire by Kate Grey
Glaciers by Alexis Smith
Postcards to America by Patrick Ingle
The Man Who Was Jekyll and Hyde by Rick Wilson
A Wizard of Earthsea by Ursula K. Le Guin
The Elementalist : Next of Kin: The Kothian Chronicles by Andrew Wood
The Misfortunes of Others by Gloria Dank
Not That Sort of Girl by Mary Wesley