Pediatric Primary Care Case Studies (65 page)
Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics

Studies have shown a relationship between parental smoking and childhood asthma. There seems to be an increased risk of early onset asthma in children exposed to tobacco smoke with an increased incidence of wheezing until age 6 years (Strachan & Cook, 1998; Weitzman, Gortmaker, Walker, & Sobol, 1990). The National Health Interview Survey (NHIS) data collected in 1981 show an increased risk of asthma in children under the age of 5 whose mothers smoked at least one half pack of cigarettes per day (odds ratio 2.1,
P =
0.001) (Weitzman et al., 1990). In addition, the American Academy of Pediatrics (1997) policy statement on the hazards of environmental tobacco smoke to children’s health clearly documents the particularly deleterious effect of tobacco smoke on children’s lungs. This policy statement notes the negative effect that parental smoking has on both the frequency of exacerbations and the severity of asthma symptoms in their children. Furthermore, when parents reduce the secondhand smoke exposure to their children, the child’s asthmatic symptoms are not as severe.
Pathophysiology of Asthma
Asthma is a chronic inflammatory disease characterized by episodic and reversible symptoms. The impact of respiratory infections on asthma incidence is an area of debate. The hygiene hypothesis, proposed by Strachan (1989), is based on the concept that immune responses are mediated by two types of lymphocyte populations: T-helper 1 and T-helper 2 cells. T-helper 1 lymphocytes produce interferon-γ and interleukin-2, and T-helper 2 lymphocytes produce interleukins that can lead to the development of IgE-mediated atopy and allergy. The exposure to airway infections and allergens early in life promotes the maturation of T-helper 1 lymphocytes over T-helper 2 lymphocytes, thereby decreasing the risk of developing allergic conditions (Gore & Custovic, 2005). Persons living in more rural environments may be exposed to allergens early in life with the development of increased T-helper 1 lymphocyte population and less atopy and asthma. There have been several studies supporting this theory as well as studies contradicting these findings (McDonnell et al., 1999; Strachan, Butland, & Anderson, 1996). The varied conclusions may be a result of the intensity, the timing, and the duration of the exposure. The underlying genetic susceptibility of the individual may also contribute to whether a particular exposure in childhood leads to the development of asthma later in life (King, Mannino, & Holguin, 2004). The most frequently cultured infectious pathogens in asthmatics undergoing bronchoscopy with bronchoalveolar lavage are viruses (adenovirus, parainfluenza, influenza, and respiratory syncytial virus),
Mycoplasma pneumoniae
, and
Chlamydia pneumoniae
(Kraft, 2000; Martin et al., 2001; McDonald, Schoeb, & Lindsey, 1991).
Asthma has been suspected to have a strong genetic component, with studies demonstrating increased prevalence of asthma among first-degree relatives of asthmatic subjects (20–25%) versus a general population prevalence
(of 4%) (Sandford, Weir, & Pare, 1996; Scirica & Celedon, 2007; Sibbald & Turner-Warwick, 1979). Asthma is regarded as a “complex” disease (i.e., one shaped by many genes and environmental factors that interact to determine susceptibility). The components of the asthma phenotype are passed down through families in complex patterns, but the genes responsible for these inherited components have not yet been identified. The disease appears to result from gene–environment and/or gene–gene interactions; however, it is unknown how many genes may be involved in asthma susceptibility and the strength of their effects. Another possibility is that a large number of genes can contribute to the development of asthma in a population, but that a small subset of genes may shape the disease in affected individuals.
The pathophysiology of asthma involves the following components:
• Airway inflammation
• Intermittent airflow obstruction
• Bronchial hyperresponsiveness
Some of the principal cells identified in airway inflammation include mast cells, eosinophils, epithelial cells, macrophages, and activated T lymphocytes. T lymphocytes play an important role in the regulation of airway inflammation through the release of numerous cytokines (see
Figure 17-1
). Airflow obstruction can be caused by a variety of changes, including acute bronchoconstriction, airway edema, chronic mucous plug formation, and airway
remodeling. Acute bronchoconstriction is the consequence of immunoglobulin E–dependent mediator release upon exposure to aeroallergens and is the primary component of the early asthmatic response. Airway edema occurs 6–24 hours following an allergen challenge and is referred to as the late asthmatic response. Chronic mucous plug formation consists of an exudate of serum proteins and cell debris that may take weeks to resolve. Airway remodeling is associated with structural changes due to long-standing inflammation and may profoundly affect the extent of reversibility of airway obstruction (Busse, O’Bryne, & Holgate, 2006).
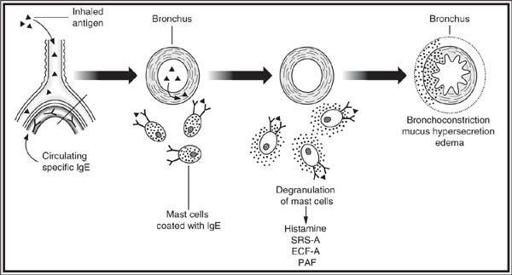
Figure 17-1 Key elements of the pathophysiology of asthma.
From Busse, W. W., O’Bryne, P. M., Holgate, S. T. (2006). Asthma pathogenesis. In: N. F. Adkinson, Jr., J. W. Yunginger, W. W. Busse, B. S. Bochner, S. T. Holgate, F. E. R. Simons, (Eds.),
Middleton’s allergy: Principles and practice
, (6th ed., Chapter 66). St. Louis, MO: Mosby. Used with permission.
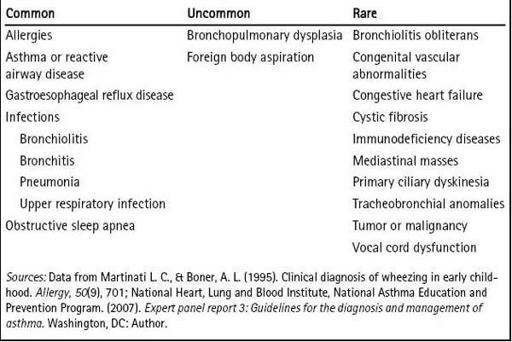
Other Common Causes of Wheezing in Children
Classically, with an acute asthma exacerbation, the child presents with wheezing and respiratory distress. Bronchospasm can also present as cough, chest pain, shortness of breath, and fatigue with exertion.
Asthma is the most likely cause of recurrent wheezing in children younger than 5 years. The most common causes of wheezing in young children are asthma, allergies, gastroesophageal reflux disease, infections, and obstructive sleep apnea. Response to bronchodilators may help differentiate asthma from other causes of wheezing. Chest radiography should be performed in children with recurrent wheezing or a single episode of unexplained wheezing that does not respond to bronchodilators. (See
Table 17-1
.)
Table 17–1 Causes of Wheezing in Children and Infants
Infant Wheezers
Many infants wheeze early in life. Risk factors for persistent wheezing and a predisposition to asthma include:
• Frequent symptoms in the first 12 months of life
• Eczema
• Elevated IgE levels
• Maternal history of asthma
• Maternal smoking
Child Wheezers
More than 85% of wheezing episodes in children are triggered by viral infections. The prevalence of asthma in school-age children in the United States is now estimated to be 9%, having doubled in about 20 years. Wheezing is extremely common, occurring in at least 50% of children, but in the absence of dyspnea or effects on sleep or activities, wheezing is not likely to be caused by asthma. Wheezing in early childhood is associated with bronchial hyperreactivity and reduced lung function in later life, and may be a reason for early intervention and maintenance medication. Children who have severe intermittent wheezing usually develop atopy. There also are transient wheezers, who usually clear by age 3, and nonatopic wheezers who do not seem to develop later asthma, although they may continue to wheeze occasionally when older.
Suspicion of asthma is increased when any one or several historical factors are present (Bush, 2007; Graham, 2006):
• Three or more episodes of otitis media (1.5 times increased risk)
• Pneumonia (1.8 times increased risk)
• Atopic dermatitis (1.9 times increased risk)
• Family asthma history (2 times increased risk)
• Laryngotracheitis (2 times increased risk)
• Allergic rhinitis (2.2 times increased risk)
• Any wheezing in first 3 years (3.3 times increased risk)
• Sinusitis (3.5 times increased risk)
• Family sinusitis history (3.9 times increased risk)
• Recurrent wheezing in first 3 years (4.7 times increased risk)
• Recurrent wheezing in years 4 through 6 (15 times increased risk)
The disease process is variable both from person to person and in each person from episode to episode. At one extreme, sufferers are continuously ill and are frequently in and out of the hospital; at the other extreme symptoms are rare, intermittent, often mild, and sometimes unrecognized. Milder symptoms of asthma often blend into those of allergic bronchitis that often accompanies allergic rhinitis (Akinbami & Schoendorf, 2002; Hopp et al., 1988). This variation can make diagnosis of certain patients extremely challenging, and the history and physical exam should be tailored to exclude other causes of wheezing, as listed earlier.
Despite the myriad causes of wheezing in children, presumptive clinical diagnosis usually is possible by obtaining a thorough clinical history and examination.
What physical examination data do you want to collect?
On physical examination, James has a nonproductive cough and some audible wheezing. His height is at the 45th percentile and his weight is at the 50th percentile with a body mass index of 17 placing him just below the 85th percentile. He is afebrile with a heart rate of 92 and a respiratory rate of 24 with mild accessory muscle use but no retractions. His oxygen saturation on room air is 92%. His head, eyes, ears, nose, and throat examination is normal except for boggy turbinates with some clear rhinorrhea and slight postnasal drainage. His tone of his voice is normal with no hoarseness noted; no visible caries nor dental erosion noted and his neck is supple with full range of motion and no lymphadenopathy. On ausculation of his lungs there are expiratory wheezes in all lung fields and an increased expiratory phase. Overall air movement is good. James’s cardiac exam reveals a regular rate and rhythm without murmurs or gallops. Radial and femoral pulses are 2+ bilaterally. The abdomen is scaphoid with good bowel sounds and there is no tenderness to palpation, masses, or hepatosplenomegaly. The remainder of the physical exam is normal.
Should you do diagnostic studies?

