Pediatric Examination and Board Review (243 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

19.
“Growing pains” is a diagnosis commonly given to children with musculoskeletal pain. All of the following are true about this entity except
(A) it most commonly involves the lower extremities, often with cramping discomfort behind the knee, in the calves, thighs, or along the tibiae
(B) the pain often awakens the child in the middle of the night and may be associated with increased activity the day before
(C) acute-phase reactants are normal
(D) these children often have morning stiffness and achiness
(E) treatment includes massage and reassurance to the parents
Match each entity that is associated with joint symptoms in questions 20 through 28 with one descriptive characteristic A through I.
20. | (A) mutation of gene encoding for pyrin |
21. | (B) conjunctivitis and positive arthritis urethritis |
22. | (C) vesiculopustular lesions on extremities and tenosynovitis |
23. | (D) resolves by 6-12 weeks |
24. | (E) nail pitting and fever dactylitis |
25. | (F) erythema chronicum migrans |
26. | (G) arthritis may precede abdominal symptoms |
27. | (H) erythema marginatum |
28. | (I) rheumatoid nodules, disease scleritis and vasculitis |
ANSWERS
1.
(B)
Systemic arthritis is the most likely diagnosis in a child with a daily spiking fever. Known as a quotidian fever, this fever pattern is characterized by 1 or 2 daily spikes higher than 102.2°F (39°C) with a rapid return to baseline (98.6°F [37°C]) or below for the rest of the day. The fever spike classically occurs in the late afternoon or evening hours, but it can occur any time of day. The child often appears well when afebrile.
Systemic arthritis is 1 of 3 types of arthritis included in the juvenile rheumatoid arthritis (JRA) classification system:
• Systemic onset
• Pauciarticular (or oligoarticular): 4 or fewer joints involved
• Polyarticular: 5 or more joints involved
• Rheumatoid factor negative
• Rheumatoid factor positive
In 1998, a new classification was proposed for chronic childhood arthritis. It also includes systemic arthritis as one of the categories, along with several other types of childhood arthritis that were not included in the JRA classification. This new nomenclature is juvenile idiopathic arthritis (JIA), and the new classification is
• Systemic
• Oligoarthritis: persistent
• Oligoarthritis: extended (progression in number of joints involved to 5 or more, occurring 6 or more months after initial diagnosis)
• Polyarticular: rheumatoid factor negative
• Polyarticular: rheumatoid factor positive
• Psoriatic arthritis
• Presence of arthritis and psoriasis
or
• Presence of arthritis and at least 2 of the following: dactylitis, nail abnormalities, psoriasis in a first-degree relative
• Enthesitis-related arthritis:
• Presence of arthritis and enthesitis
or
• Presence of either arthritis or enthesitis with at least 2 of the following: positive HLA-B27; onset of arthritis in male more than 8 years of age; sacroiliac or inflammatory back pain; +ve family history (ankylosing spondylitis, enthesitis-related arthritis; sacroiliitis with inflammatory bowel disease; reactive arthritis or acute anterior uveitis in a first- or second-degree relative)
• Undifferentiated arthritis (fits no other category, or fits into more than 1 category)
This newer classification system includes the 2 spondyloarthropathies, specifically enthesitisrelated and psoriatic arthritis. The JIA system should increase the homogeneity of the subgroups of childhood arthritis patients, which should promote improved recognition of the disease presentation, course, response to treatment, and long-term outcomes of each arthritis subgroup. Research projects, such as studies on disease pathogenesis or genetic markers, may yield more information and result in changes to the classification system in the future. Literature published after 1998 often refers to JIA instead of JRA.
2.
(A)
The CBC in active systemic arthritis usually has a marked elevation of the leukocyte count (can be >30,000/mm
3
) and platelets (frequently >500,000/mm
3
), as well as anemia (hemoglobin often <10 g/dL). Low normal or below normal platelet counts should raise concern of malignancy, especially leukemia, which can present with clinical and laboratory features (eg, hepatosplenomegaly, lymphadenopathy, joint pain, fevers, anemia, and increased erythrocyte sedimentation rate) similar to those seen in systemic arthritis. (Note: A rare complication of systemic arthritis, macrophage activation syndrome [MAS], is associated with depressed platelet levels. This acute illness is characterized by disseminated intravascular coagulation, purpura, hepatic failure, encephalopathy, and other features. MAS has a high mortality rate if not treated rapidly and aggressively. High-dose intravenous CS are the first line of treatment.) Children with systemic arthritis almost always have a negative ANA.
3.
(A)
The classic systemic rash is migratory and so evanescent that it resolves within a few hours or less (
Figure 140-1
). There is no need (nor time!) to biopsy it. This precipitous resolution of the rash would not be expected in a leukocytoclastic vasculitis lesion. The systemic rash is usually more prominent during the fever spikes. It appears most often on the trunk and extremities but may be present also on the face, palms, and soles. It may occasionally be pruritic.

FIGURE 140-1.
Evanescent salmon-colored, macular, or maculopapular rash of systemic arthritis. See color plates.
4.
(C)
Eye involvement, common in other subtypes of childhood arthritis, is typically absent in systemic arthritis. Extra-articular features include the quotidian fever and evanescent rash previously described, as well as polyserositis, hepatosplenomegaly, lymphadenopathy, pneumonitis, and anemia of chronic disease.
5.
(C)
The first-line medication for systemic arthritis is a NSAID, such as ibuprofen (35-40 mg/kg per day; maximum dose of 2400 mg/day) or naproxen (15-20 mg/kg per day; maximum dose of 1000 mg/day), both of which are approved for children and available in liquid form. Note that anti-inflammatory doses are higher than those recommended for analgesia and antipyrexia. Other NSAIDs approved for children include tolmetin, diclofenac, and sulindac, as well as indomethacin, which may control fevers and polyserositis symptoms better than other NSAIDs but frequently causes epigastric pain and headaches. CS are often used to treat systemic features not responding to NSAIDs. Before starting CS treatment, the physician must be certain that no other diagnosis, such as leukemia, is being overlooked. Methotrexate may help decrease systemic symptoms and is often effective in treating active joint inflammation. Methotrexate is approved for and commonly given to children with systemic and other JIA subtypes who have persistent arthritis despite NSAID treatment. Antitumor necrosis factor alpha (anti-TNF alpha) drugs, the first class of biologics to be used widely for treatment of rheumatoid arthritis, are used to treat active joint disease in children that has not responded adequately to methotrexate. This class of medication may be less efficacious in systemic arthritis compared with other subtypes of childhood arthritis. Five anti-TNF alpha medications are available: etanercept, adalimumab, infliximab, golimumab, and certolizumab pegol; only the first 2 are approved for use in JIA. The biologic medications are targeted therapies. Many of them directed against proinflammatory cytokines and are used in several diseases including JIA, adult rheumatoid arthritis, inflammatory bowel disease, psoriasis, SLE, severe uveitis, Behçet, sarcoidosis, and various vasculitides, although their use is often off-label. Two of the anticytokine biologics, anti-interleukin (IL)1 (anakinra; canakinumab), and anti-IL6 (tocilizumab) appear to have special efficacy in treating systemic features of systemic JIA. Many of the biologic medications are in phase 2/3 testing in pediatric and adult rheumatic diseases.
6.
(A)
Although systemic CS are effective in controlling systemic features and usually decrease joint pain and swelling, they do not halt the progression of the joint disease and destruction in childhood arthritis.
7.
(D)
Liver enzymes should be monitored regularly (every 1-2 months) in patients on methotrexate therapy. The concern for significant hepatotoxicity in patients with high cumulative methotrexate doses after years of treatment does exist but has yet to be substantiated in studies evaluating liver biopsies in these patients. Alcohol consumption is contraindicated in patients on methotrexate. Other complications of low-dose weekly methotrexate include marrow toxicity, which is generally mild and reversible, as well as mouth sores and nausea. Supplementation with folic acid may decrease these side effects. Immunosuppression tends to be mild at the low methotrexate doses given for childhood arthritis, so severe or opportunistic infections rarely occur. The infection risk may be increased if the child is also receiving CS. It is recommended that children on methotrexate not be immunized with live attenuated vaccines. Methotrexate is highly teratogenic; therefore, patients who are sexually active must use effective birth control methods while on this medication.
8.
(E)
Delayed growth, short stature, and osteoporosis are attributable to chronic illness, CS treatment, and poor nutrition. Decreased weightbearing and limited participation in physical activities contribute further to the osteoporosis. Micrognathia develops in many patients and may cause chewing difficulties, orthodontic problems, and even obstructive sleep apnea. Patients with significant cervical spine arthritis that results in C1-C2 instability or ankylosis of posterior vertebral processes are at risk for spinal cord injury (
Figure 140-2
). Functional disabilities historically occurred in 15-30% of children; however, with early aggressive treatment and the availability of biologic medications, the prognosis has improved greatly.
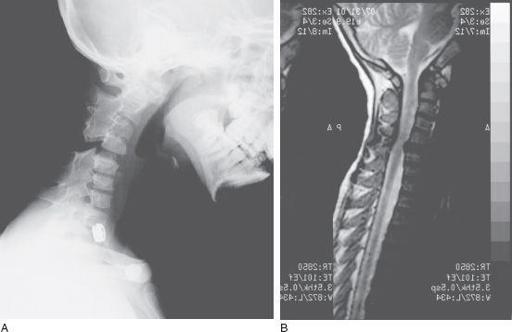
FIGURE 140-2. A.
Cervical spine radiograph showing fusion of the spinous processes of C2-C4 and C5-C7 in a 9-year-old boy with systemic arthritis since 18 months of age.
B.
MRI of the same patient showing cervical cord impingement at the C4-C5 level; note that impingement is only at the cervical level which is not fused and where all neck flexion and extension takes place.
