Pediatric Examination and Board Review (240 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

14.
(A)
All types of Niemann-Pick disease (A-D) are transmitted in an autosomal recessive inheritance pattern.
15.
(A)
Gaucher disease is most common among Ashkenazi Jews and is one of the most frequent lysosomal disorders. The deficient enzyme is betaglucocerebrosidase. Glucosylceramide accumulates in various tissues: brain, spleen, bone marrow, and liver.
16.
(E)
Children with Tay-Sachs disease present with hyperacusis and a propensity to startle with noise. Patients can have myoclonic seizures and a “cherry red spot” (see
Figure 138-2
) on fundoscopic examination. The disorder is transmitted in an autosomal recessive fashion, especially among those of Ashkenazi Jewish descent. The deficient enzyme is hexosaminidase A.
17.
(D)
Approximately 80% of patients with metachromatic leukodystrophy develop symptoms in the first 2 years of life. Symptoms include ataxia, neuropathy, optic atrophy, seizures, and spasticity. Loss of speech, intellect, and coordination are also observed. The enzyme deficiency is arylsulfatase A.
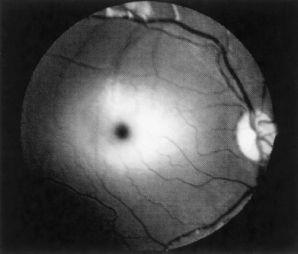
FIGURE 138-2
.
Retinal cherry-red spot in a patient with Tay-Sachs disease. The whitish ring surrounds the dark macula. (Reproduced, with permission, from Lichtman MA, Beutler E, Kipps TJ, et al. Williams Hematology, 7th ed. New York: McGraw-Hill; 2006: Fig. 73-4.)
18.
(B)
Methyl-CpG-binding protein 2 (MeCP2) most likely regulates gene expression and chromatin structure by binding to methylated DNA. This gene is mutated in most cases of sporadic Rett syndrome.
19.
(C)
Krabbe disease or globoid cell leukodystrophy is caused by a deficiency of the lysosomal hydrolase, galactocerebroside beta-galactosidase.
 S
S
UGGESTED
R
EADING
Crumrine PK. Degenerative disorders of the central nervous system.
Pediatr Rev.
2001;22:370-379.
Neul JL, Zoghbi HY. Rett syndrome: a prototypical neurodevelopmental disorder.
Neuroscientist.
2004;10:118-128.
Osborn AG. Inherited metabolic, white matter and degenerative diseases of the brain. In: Osborn AG, ed.
Diagnostic Neuroradiology
. St. Louis, MO: Mosby; 1994:716.
Swaiman KF, Wu Y. Cerebral palsy. In: Swaiman KF, Ashwal S, Ferriero DM, eds.
Pediatric Neurology
:
Principles
&
Practice.
4th ed. Philadelphia, PA: Mosby; 2006:491.
CASE 139: A 17-YEAR-OLD BOY WITH WEAKNESS AND PARESTHESIAS
You are called to the ED to evaluate a 17-year-old young man who presents with upper and lower extremity weakness and back pain. The patient states that he was in his usual state of health until approximately 2
1
/
2
weeks ago when he developed an upper respiratory tract infection. His primary doctor thought the infection was most likely due to a virus. Yesterday the patient states he experienced tingling over the soles of his feet. His gait became unsteady and his legs “felt weak.” On awakening this morning, the patient states the weakness had spread to his arms. His lower extremities are also weaker compared with the previous day, and he cannot walk 5 meters without support. There is no history of trauma. The patient states he has had a hard time urinating.
On physical examination, the patient is an athleticappearing young man in mild distress. He is afebrile with a heart rate of 124 bpm. His blood pressure seems to fluctuate. His mental status and cranial nerve examination are normal. On motor examination, he has normal tone and bulk. He is barely able to lift his legs from the bed and cannot move his toes. He is barely able to move his arms against gravity. His deep tendon reflexes are absent bilaterally in the lower extremities and 1/4+ in the upper extremities. Sensation to vibration and pinprick are slightly diminished in the lower extremities.
SELECT THE ONE BEST ANSWER
1.
In evaluating this patient further, which of the following studies could help in confirming the diagnosis?
(A) MRI of the spine
(B) lumbar puncture
(C) nerve conduction velocities
(D) EMG
(E) all of the above
2.
An MRI of the spine is performed with and without contrast. The study is unremarkable. CSF examination in this patient is most likely to reveal which of the following?
(A) elevated opening pressure, elevated protein, normal glucose, and a cell count of about 300 lymphocytes/mm
3
(B) normal opening pressure, normal protein and glucose, and a cell count of about 10 leukocytes/mm
3
(C) normal opening pressure, elevated protein, normal glucose, and a cell count of about 10 mononuclear cells/mm
3
(D) elevated opening pressure, elevated protein, decreased glucose, and about 1000 polymorphonuclear cells/mm
3
(E) no abnormal CSF findings
3.
Clinical features of Guillain-Barré syndrome (GBS) include all of the following except
(A) fever at onset
(B) weakness involving more than 1 limb
(C) areflexia
(D) nearly symmetric physical signs
(E) cranial nerve involvement
4.
The Moro reflex should disappear by what age?
(A) 1 month
(B) 2 months
(C) 6 months
(D) 12 months
(E) 15 months
5.
The tonic neck reflex should disappear by what age?
(A) 1 month
(B) 6 months
(C) 12 months
(D) 15 months
(E) 18 months
6.
The palmar grasp reflex should disappear by what age?
(A) 1-2 months
(B) 3-6 months
(C) 6-9 months
(D) 9-12 months
(E) the palmar reflex disappears at the same time as the plantar grasp reflex
7.
On average, by what age will a child mimic housework according to the Denver Developmental Screening Test (Denver II)?
(A) 15 months
(B) 2 years
(C) 3 years
(D) 4 years
(E) 6 years
8.
Which of the following therapies are used in the treatment of GBS?
(A) plasmapheresis
(B) IVIG
(C) high-dose corticosteroids
(D) A and B
(E) A, B, and C
9.
The differential diagnosis of GBS includes all of the following diagnoses except
(A) porphyria
(B) botulism
(C) HIV infection
(D) hysteria
(E) no exception; all of the above are in the differential
10.
Which of the following statements regarding GBS is false?
(A) in children, acquired inflammatory neuropathy (GBS) is the most frequent cause of peripheral nerve disease
(B) for the most part, males and females are equally affected
(C) surgery has been shown to be a cause of GBS
(D) sensory symptoms are more common than weakness
(E) GBS occurs in all parts of the world
11.
Which of the following is (are) a complication(s) of plasmapheresis?
(A) hypocalcemia
(B) hemorrhage
(C) transfusion reaction
(D) septicemia
(E) all of the above
12.
Which of the following heavy metals is associated with neuropathy, alopecia, and GI symptoms?
