Pediatric Examination and Board Review (235 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

5.
(E)
Pseudotumor cerebri, or idiopathic intracranial hypertension, is characterized by increased intracranial pressure without evidence of a brain tumor or mass lesion as the cause of elevated pressure. Patients typically present with headaches, papilledema, visual field defects (typically an enlarged blind spot), and, occasionally, diplopia. There is no gender predilection in early childhood. An important risk factor for pseudotumor cerebri is obesity. Other risk factors include various drugs, such as oral contraceptives, high levels of vitamin A, and corticosteroids, which the patient should avoid if possible. Steroid use can also play a role in weight gain. In terms of treatment, weight reduction is strongly recommended in those patients who are obese. A drop in body weight by 15% may even lead to resolution of symptoms, including elevated intracranial pressure. Given this patient’s visual symptoms she should not drive until her vision has been restored. Finally, given the daily use of analgesics, this patient is at risk for developing a medication overuse headache, formerly known as rebound headaches. Patients with medication overuse headaches usually see their primary headache disorder (eg, migraines or pseudotumor cerebri) transformed into chronic daily headaches. Once medication overuse headaches develop, they can be very difficult to treat, and patients may also develop a comorbid depression. Patients usually need to be detoxified for approximately 2 weeks. Because the headaches may be severe, some patients may require hospitalization. Other treatment strategies have been reported.
6.
(C)
Each of the drugs listed in this question have been used in the treatment of migraines. However, acetazolamide has been shown to decrease the formation of CSF. Acetazolamide is a sulfonamide drug. Thus, for those patients who are allergic to sulfonamides, furosemide may be used for a similar purpose. Other side effects of acetazolamide include drowsiness, numbness, renal calculi, and anorexia. Incidentally, patients with pseudotumor cerebri and obesity should avoid valproic acid (if clinically possible) because this medication may also cause weight gain.
7.
(C)
The mean head circumference for a full-term newborn boy at birth is approximately 35 cm; it is 34 cm for girls.
8.
(C)
Migraines without aura are the most common type of migraine in children and adolescents. When evaluating a patient with headaches it is important to note the temporal pattern to the headache. The examiner should ascertain whether the headache is acute versus chronic, single versus recurrent, or progressive versus nonprogressive. At times, the physician may observe a mixed pattern. This question gives an example of an acute recurrent headache. Typically, acute recurrent headaches, separated by pain-free intervals and associated with nausea, vomiting, photophobia, or phonophobia, are a result of migraines. Because this patient does not have an aura before the headache it would be classified as migraine without aura. Patients with complicated migraine typically have a transient neurologic deficit associated with their headache. This deficit could include weakness or sensory loss. However, complicated migraine is a diagnosis of exclusion, and, as a result, a structural lesion should be ruled out by neuroimaging. Basilar migraines typically present with symptoms referable to the brainstem, cerebellar, or other posterior circulation territories. These symptoms include blurred vision, vertigo, ataxia, dizziness, paresis, dysarthria, nausea, and vomiting. It is more common among adolescent females.
9.
(A)
This is an example of classic migraines or migraines with aura. The headaches are acute and recurrent with pain-free intervals. The patient can describe the aura as brightly colored lights and does not appear to lose consciousness during the episode, thus ruling out complex partial seizures. Patients with ophthalmoplegic migraines complain of severe pain located behind the eye. They also present with a complete or incomplete third cranial nerve palsy (eg, ptosis, diplopia, lateral eye deviation, and mydriasis), which may persist for several days even after the headache has subsided.
10.
(A)
When a patient without a history of severe headaches complains of the “worst headache of his or her life” in the setting of meningismus and emesis, the clinician should consider a diagnosis of subarachnoid hemorrhage (see
Figure 136-4
). In this case, a head CT can be performed relatively quickly to evaluate this possibility. Certainly, a neuroimaging study would be performed before lumbar puncture. Intracranial hemorrhage, stroke, and seizures have been reported following cocaine use. As a result, a urine toxicology screen may be an appropriate study in the evaluation of this patient. In terms of the next appropriate action, a neuroimaging study would enable the physician not only to confirm the diagnosis but also to assist in further managing the patient should he or she need a neurosurgical consultation or neuro-intensive care.
11.
(D)
Subarachnoid hemorrhages may be difficult to appreciate on head CT (see
Figure 136-5
). A more definitive test may be the lumbar puncture. In patients with subarachnoid hemorrhage, the CSF may contain red blood cells that do not clear in serially collected samples. In addition, xanthochromia may be seen as early as 4 hours after the bleed. Subarachnoid hemorrhages can be seen following head trauma, meningitis, birth trauma, and coagulopathies. However, the most likely etiology is a vascular malformation, although these are exceedingly rare in very young children. Patients with complicated migraine should not have red blood cells or xanthochromia on lumbar puncture. Subdural hematoma, hemorrhagic herpes meningoencephalitis, and glioblastoma multiforme are typically suggested by abnormalities observed with head CT.
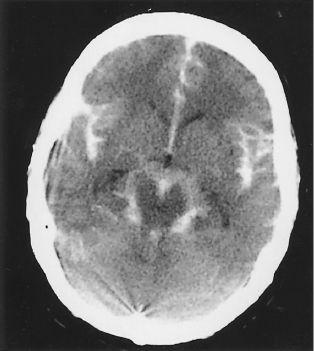
FIGURE 136-4
.
A non-contrast head CT demonstrating diffuse subarachnoid blood. (Reproduced, with permission, from Stone CK, Humphries RL. Current Diagnosis & Treatment: Emergency Medicine, 6th ed. New York: McGraw-Hill; 2008: Fig. 35-1.)
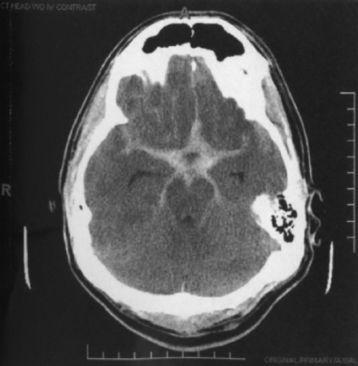
FIGURE 136-5
.
Classic appearance of a large subarachnoid hemorrhage. Notice the hemorrhage pattern fills the cerebrospinal fluid spaces at the base of the brain and around the brain stem. (Reproduced, with permission, from Doherty G. Current Diagnosis & Treatment: Surgery, 13th ed. New York: McGraw-Hill; 2010: Fig. 36-22.)
12.
(E)
Treatment of migraines involves both pharmacologic and nonpharmacologic methods. The patient first needs to be assured that he or she does not have a serious or life-threatening condition. The clinician should always start with nonpharmacologic methods in the treatment of migraines. This includes recognition and elimination of triggering factors, such as relaxation methods to reduce stress, adequate sleep, and a regular diet. In terms of pharmacologic therapy, prophylactic agents can be used should nonpharmacologic methods fail and the patient continue to experience frequent headaches. Typically, this type of patient has severe headaches and misses several days of school. Some commonly used prophylactic drugs include amitriptyline, valproic acid, propranolol, and cyproheptadine.
13.
(D)
Hemicrania continua is an example of an indomethacin-responsive headache. This headache consists of severe, steady pain localized to one side of the head. The patients are usually female without a family history of such headaches.
14.
(C)
This question highlights several of the classes of medications used in the prophylactic treatment of migraine headaches. Sumatriptan is an example of a 5-HT receptor agonist.
15.
(E)
Menstruation, certain foods, fatigue, and stress are common triggers of migraines. Other triggers include oral contraceptive pills, anxiety, physical exertion, alcohol, sleep deprivation, and weather changes.
16.
(B)
The 3 most common primary brain tumors in children are, in order of decreasing frequency, supratentorial low-grade astrocytoma, medulloblastoma, and cerebellar astrocytoma.
17.
(B)
Medulloblastomas are posterior fossa tumors typically occurring in the midline. They tend to be well-demarcated tumors. Cyst formation, hemorrhage, and calcifications are rare in comparison with cerebellar astrocytomas. Some studies have suggested that the presence of the
c-myc
oncogene is associated with a poorer prognosis. Brainstem gliomas tend to occupy the region of the brainstem near the fourth ventricle and aqueduct of Sylvius. Thickening of the pons is often observed. Ependymomas can occur anywhere along the ventricular system. Most of the tumors (two-thirds) are infratentorial. Ependymomas are well defined and can be very cystic. Meningiomas are relatively uncommon tumors in children. When they are observed, they tend to occur in the posterior fossa or in the ventricular system, often causing obstructive hydrocephalus. This question highlights the importance of recognizing chronic progressive headaches, which usually imply some pathologic process, such as brain tumor, pseudotumor cerebri, subdural hematoma, or hydrocephalus, to name a few. In general, migraine headaches are rare in patients younger than 5 years.
18.
(A)
In contrast to medulloblastomas, cerebellar astrocytomas can occur anywhere in the cerebellum. Most of these tumors are cystic, as shown in this example. In some cases, a solid mural nodule is associated with a large cyst. Calcifications are seen in a quarter of the patients. Cerebellar astrocytomas can be separated into 2 groups: diffuse astrocytoma and juvenile cerebellar astrocytoma. Most of the astrocytomas fall into the latter category. Juvenile cerebellar astrocytoma, shown in this example, is cystic and associated with better survival rates than the diffuse type.
19.
(E)
Choroid plexus tumors, colloid cysts, giant cell astrocytomas, and meningiomas are all examples of ventricular tumors. This figure (
Figure 136-2
) shows a choroid plexus papilloma involving the lateral ventricle, a typical site for this tumor in older children. These tumors are usually found in the fourth ventricle in very young children and adults. Unlike colloid cysts, which are found in the third ventricle, choroid plexus tumors are rarely seen in the third ventricle. Patients with choroid plexus tumors often present with signs of increased intracranial pressure, such as vomiting and headache. Subependymal giant cell astrocytomas occur in the region of the ventricles and are often associated with TSC. They are commonly seen in the area around the foramen of Monro.
 S
S
UGGESTED
R
EADING
