Pediatric Examination and Board Review (198 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) streptococcal skin infections are not painful
(E) group A beta-hemolytic streptococci can cause balanitis and vulvovaginitis
17.
Anal dilation is a concerning finding for suspected child sexual abuse. Which of the following is false?
(A) stool in the vault can cause anal dilation
(B) a history of encopresis can be associated with anal dilation
(C) a child who has been in the knee-chest position for more than 30 seconds may have a dilated anal opening
(D) digital examination of the anus most often is the method that can elucidate if there has been acute trauma
(E) venous congestion is a normal finding on anal examination
18.
Which is a true statement regarding the role of the pediatrician in child sexual abuse evaluations?
(A) each state has it own standards with regard to when a pediatrician must report a suspected case
(B) pediatricians are advised to keep minimally detailed documentation in reported cases because, in court, information may be used to discount the doctor’s findings
(C) the more explicit the record keeping the less likely a physician may have to testify in civil court where the legal standard for evidence is “preponderance of evidence”
(D) if a pediatrician is concerned that a child is sexually abused based on a behavioral change (eg, new-onset enuresis in a 6-year-old) or a nonspecific physical finding (eg, labial adhesion or vaginal rash), he or she is mandated to report their concern to regional authorities
(E) referral to a child advocacy center or regional multidisciplinary teams should only occur when there is sufficient physical evidence to support child sexual abuse
ANSWERS
1.
(D)
The next appropriate step would be to interview the caretaker and child separately to elucidate any concerns for sexual abuse. Although at this point there are multiple etiologies to consider that can cause a vaginal discharge in this age group, the topic of sexual abuse must be explored with both the child and parent. It is in the purview of the pediatrician to do an initial screening with regard to the possibility of child sexual abuse before referral to a child advocacy center or specialists in the area of child sexual abuse. The discharge from vulvovaginitis is not usually blood-tinged or malodorous, and topical treatment without examination is inappropriate.
2.
(E)
In most of the cases of labial adhesions, vaginal bleeding is not the primary presenting clinical feature.
3.
(A)
Genital examination of the prepubertal child should have the caretaker in the room in most circumstances to provide support for the patient. Examination rarely should require sedation, and attempts before the examination to explain it often helps the child to be cooperative. The physician should ensure that he or she can visualize the inner thighs, the labia majora and minora, clitoris, urethra and periurethral tissues, the hymen and the hymenal opening, the fossa navicularis, and the posterior fourchette (see
Figure 110-1
). Often it is advised that 2 positions be used to visualize all of the structures mentioned; both the supine frog leg position and the knee-chest prone position work well. Examining the child prone in the knee-chest position greatly enhances the examiner’s ability to visualize the posterior hymenal rim. A speculum exam is not indicated on a prepubertal child even if a foreign body is suspected.
4.
(A)
Ten percent of confirmed cases of maltreatment in children are a result of sexual abuse. Perinatal transmission of chlamydia and human papilloma virus (HPV), if detected in the newborn period, are not indicative of sexual abuse. The definition of child sexual abuse is not based on penetration; it is operationally and developmentally defined where a child engages in sexual activities he or she doesn’t understand, is not developmentally prepared for, and cannot give consent. These acts violate social taboos and are proscribed by society’s standards not parental standards.
5.
(B)
A fimbriated hymen is a normal variant. Most children who are sexually abused have a normal examination without sign of trauma, scarring, obvious bleeding, and/or discharge. Our current examination standards do not focus on the diameter of the hymenal opening but on findings specific to the hymenal ring and surrounding structures. Straddle injuries rarely involve the hymen but usually affect more lateral anatomic structures.
6.
(E)
All girls are born with a hymen; congenital absence of the hymen has not been described.
7.
(C)
Any child with a malodorous or blood-tinged discharge deserves a thorough examination, which may require anesthesia. The medical provider must ensure that a timely assessment occurs to assess for injury, foreign body, or infection. How emergently this happens is dictated by the seriousness of the child’s condition and level of concern for child sexual abuse. Emergent referral is required to ensure timely collection of evidence and the performance of a thorough and child-focused examination by a medical professional skilled in the area of child sexual abuse evaluation and treatment.
8.
(B)
Urethral prolapse most often occurs in African American females. A common presentation is vaginal bleeding or spotting. Most of the time urethral prolapse is not associated with tenderness on examination and can be conservatively managed with sitz baths and estrogen cream if the prolapsed area is nonnecrotic.
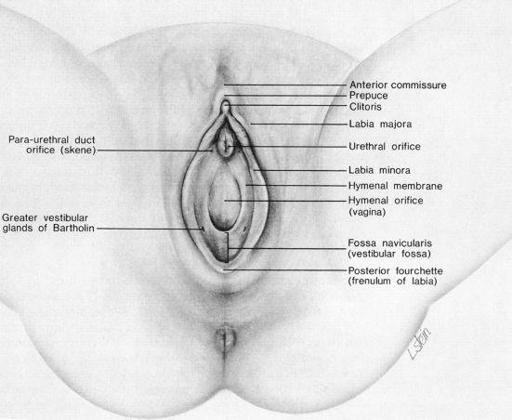
FIGURE 110-1.
External structures of the female genitalia. (Reproduced, with permission, from Finkle M, Giardino A. Medical Evaluation of Child Sexual Abuse, A Practical Guide. 2nd ed. Thousand Oaks, CA: Sage;2002:46.)
9.
(A)
This child most likely has the syndrome of recurrent abdominal pain. The pain is very real to the patient. Criteria for diagnosis include recurrent pain for more than 3 months, usually female gender, age 4-8 years, normal physical examination, growth, and laboratory testing. With the family the physician should explore detection of stressors that could underlie this entity. Treatment is supportive and obviously aimed at trying to modify any perceived stressors.
10.
(E)
The patient described in the vignette presents with a clinical picture consistent with acute PID and, possibly, perihepatitis, the Fitz-Hugh and Curtis syndrome. Bilateral lower abdominal pain and tenderness on examination, cervical motion tenderness, and adnexal tenderness may be present. There is usually a history of fever and continuous abdominal pain. Very few patients with PID have unilateral tenderness. Such a finding would warrant consideration of other etiologies such as appendicitis, ectopic pregnancy, or urinary tract disease. In general, symptomatic
N gonorrhoeae
infection is more acute than this patient’s presentation and is usually associated with menses.
11.
(B)
Liver function tests in Fitz-Hugh and Curtis syndrome, a complication of acute PID, are usually normal. The risk of tubal closure and therefore ectopic pregnancy is significant. With repeated episodes of PID, the risk of infertility increases.
12.
(A)
Nonspecific vulvovaginitis accounts for most of the vulvovaginitis seen in prepubertal girls. It is related to poor hygiene but also occurs because of the decreased estrogen level. The process is more atrophic in nature and the vulvar skin is more easily traumatized. Normal flora such as
Staphylococcus epidermidis
, alpha-hemolytic streptococci, diphtheroids, lactobacilli, and gram-negative bacteria may be isolated. Nonspecific treatment involving good hygiene, protective ointments, no harsh soaps, and sitz baths is initially tried to eradicate symptoms. Specific respiratory and enteric pathogens can cause vulvovaginitis (eg,
Streptococcus pyogenes
,
S pneumoniae
,
S aureus
, and
Shigella
species).
Candida
species are unusual unless there has been some predisposing condition (eg, recent antibiotic therapy).
13.
(D)
The presence of condyloma acuminata, anogenital warts, is suspicious for child sexual abuse if they were not perinatally transmitted. The classic lesions are irregular, multidigitated wart-like growths. Perinatal maternal-infant transmission has been documented, but the time to presentation is variable, with reports up to about 20 months of age. The mode of transmission of HPV, the wart virus, is also unclear, and the variable incubation period and subclinical presentation make it difficult to identify the contact source. Any child with the presentation of HPV infection warrants an in-depth family history and assessment for risk of child sexual abuse. A higher suspicion for child sexual abuse is warranted in children who present with new warts when older than 2 years of age.
14.
(C)
Straddle injuries to the genital region of children are common and rarely involve penetration. In accidental straddle injuries there is often a history of a fall onto an object to cause a crush injury. Characteristically the injury is localized to the labia minor and majora and rarely involves the hymenal area or posterior aspect of the fourchette. Ecchymoses on the scrotum or a minor laceration to the penis or scrotum are associated injuries in boys. Straddle injuries are rare in nonambulatory children, rarely involve major trauma, and are rarely associated with coexisting anal trauma.
15.
(B)
If there is no urinary obstruction, in addition to ongoing monitoring by the physician, topical estrogen treatment is an option.
16.
(E)
Group A beta-hemolytic streptococci can cause perianal disease, vaginitis, and balanitis. The diagnosis is made by history and culture of the throat and rectum. The culture request must indicate that group A streptococcus is suspected, so that appropriate culture techniques are used. The pain, itching, and blood-tinged stool are typical; there may also be a family history of recent streptococcal illness that could be the source of the infective organism. Nasopharyngeal carriers and autoinoculation are postulated as the mechanism by which the disease occurs. A throat culture in one study was positive 60% of the time in this type of scenario.
17.
(D)
Venous congestion is a normal finding on anal examination. Stool in the anal vault, a history of encopresis, and a child who sits in the knee-chest position for a period of time will all have normal anal dilation. A digital examination in a child who has been anally sexually abused often does not reveal any abnormal findings.
18.
(C)
In the United States all pediatricians are required by law to report suspected cases of child sexual abuse. It is highly advised that pediatricians keep detailed records of their evaluation to assist the investigational agencies and for purposes of recreating findings. The more detailed the report, the more likely that a doctor may not have to testify in civil court. Pediatricians should report cases where they have an intermediate or high index of suspicion for child sexual abuse; consultation with regional experts is always encouraged.
 S
S
UGGESTED
R
EADING
