Pediatric Examination and Board Review (201 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(C) hypoglycemia
(D) A and B
(E) A, B, and C
4.
What should be included in the initial management?
(A) surfactant administration
(B) insertion of umbilical lines
(C) sepsis workup and antibiotic administration
(D) IV maintenance fluids and a chest radiograph
(E) all of the above
5.
All of the following monitoring is required except
(A) ABGs and O
2
saturation
(B) electrolytes, calcium (Ca), and glucose
(C) BP
(D) bilirubin
(E) all of the above (no exception)
6.
The baby is under a radiant warmer and receiving a steady rate of IV fluids. The first set of serum electrolytes at 12 hours of age includes a sodium (Na) 150 mEq/mL, potassium (K) 5.8 mEq/mL, chloride (Cl) 108 mEq/ mL, and carbon dioxide (CO
2
) 18. What do you want to do?
(A) increase fluid administration
(B) decrease fluid administration
(C) increase Na concentration in the administered fluids
(D) A and C
(E) make no change and repeat electrolytes in 12 hours
7.
On day 2 of life the patient’s weight is 550 g and the urine output is 1 mL/kg per hour. The ventilatory settings are Fio
2
40%, PIP 18, PEEP 5, I-time 0.3, and a rate of 40/minute. An ABG shows a pH of 7.38, Paco
2
of 38, and a Pao
2
of 95. Serum electrolytes reveal Na 152 mEq/mL, K 5.6 mEq/mL, Cl 110 mEq/mL, CO
2
18, Ca of 6.5 mEq/mL, and bilirubin of 4.0 mg/dL. What is the next step?
(A) increase fluid administration rate and add Ca to fluids
(B) increase fluid administration rate and add Ca and K to fluids
(C) make ventilatory setting changes
(D) start hyperalimentation
(E) A, C, and D
8.
On day 3 of life the patient’s weight is 570 g and the urine output is 3 mL/kg per hour. The ventilatory settings are Fio
2
0.3, PIP 16, PEEP 5, I-time 0.3, and a rate of 30/minute. Determination of serum electrolytes reveals Na 148 mEq/mL, K 3.5 mEq/mL, Cl 108 mEq/mL, CO
2
18, and Ca 7.5 mEq/mL. What is the next step?
(A) increase IV fluids and add K
(B) administer IV fluids at the same rate and add K
(C) increase IV fluids but do not add K
(D) no change
(E) decrease total fluids
9.
On day 3 of life, the ventilatory settings have increased to Fio
2
0.5, PIP 20, PEEP 6, and a rate of 50/minute. On examination, there is an active precordium. The peripheral pulses are full; the BP is 35/16, and, on auscultation, there is a grade II/VI systolic murmur. The hematocrit is 32%. An echocardiogram confirms your diagnosis of a PDA. The best initial management of this condition is
(A) prostaglandins
(B) indomethacin
(C) furosemide
(D) increase IV fluids
(E) decrease the Fio
2
10.
Which condition is most often associated with PDA?
(A) congenital syphilis
(B) congenital varicella
(C) congenital cytomegalovirus
(D) congenital rubella
(E) congenital parvovirus B19
11.
IV indomethacin could adversely affect which of the following?
(A) urine output
(B) serum sodium
(C) serum creatinine
(D) A, B, and C
(E) none of the above
12.
After three doses of IV indomethacin, the patient improves. The ventilatory settings are Fio
2
30%, PIP 16, PEEP 5, and a rate of 30/minute. No murmur is heard. You start nasogastric feedings. After 3-4 days, the patient develops abdominal distention and has increased residual feeds. On abdominal examination the baby has some guarding. All would be appropriate actions except
(A) make the patient NPO and institute gastric suction
(B) order an abdominal radiograph
(C) order a sepsis workup
(D) start antibiotics
(E) change the enteral feeds to an elemental formula containing a probiotic
13.
The patient’s abdominal radiographs can be seen in
Figure 112-1
. What is the next step?
(A) order serial abdominal radiographs
(B) monitor the platelet count
(C) monitor the urine output closely
(D) monitor ABGs
(E) all of the above

14.
The patient in
Figure 112-2
requires surgery. What is an absolute indication for surgery in a patient with necrotizing enterocolitis (NEC)?
(A) free air
(B) fixed loop sign
(C) intractable thrombocytopenia
(D) intractable acidosis
(E) signs of peritonitis
15.
The patient’s abdominal radiograph improves during the next few days. The platelet count is stable. Which is the most likely complication of NEC?
(A) intestinal stricture
(B) chronic constipation
(C) neurodevelopmental problems
(D) increased risk of food allergies
(E) increased risk of irritable bowel syndrome
16.
What routine monitoring should be done in the first week of life in all premature babies?
(A) a head ultrasound
(B) an echocardiogram
(C) cardiac catheterization
(D) an ophthalmology examination
(E) A, B, and D
ANSWERS
1.
(B)
Antenatal corticosteroids, betamethasone, or dexamethasone decrease morbidity from respiratory distress, NEC, and intraventricular hemorrhage. Steroids are most effective if delivery occurs 48 hours to 7 days after administration, but some beneficial effect has been seen as early as 12 hours after the first dose.
2.
(E)
Premature babies lighter than 750 g and less than 28 weeks’ gestation have a very high insensible water loss. The insensible water loss is increased under a radiant warmer, in low ambient humidity, and during phototherapy. RDS is caused by surfactant deficiency. Surfactant is produced by type II alveolar cells. Surfactant decreases surface tension, thus decreasing the pressure required to stabilize the alveolus. Sepsis should always be considered in a sick newborn. Hypo- or hyperglycemia can both occur.
3.
(E)
Babies with surfactant deficiency have stiff lungs with decreased compliance; compliance of the chest wall in premature babies is high. In surfactant deficiency, a higher pressure is needed to open the alveoli; this manifests as retractions. In a premature baby, RDS or surfactant deficiency is the most likely cause of respiratory distress. Sepsis should always be considered in a baby with respiratory distress. Hypoglycemia can also present as respiratory distress.
4.
(E)
Surfactant is 90% lipid and 10% protein. Surfactant proteins A, B, C, and D are important for dispersion of surfactant. Exogenous surfactant is administered via an endotracheal tube. Synthetic and natural surfactants are available.
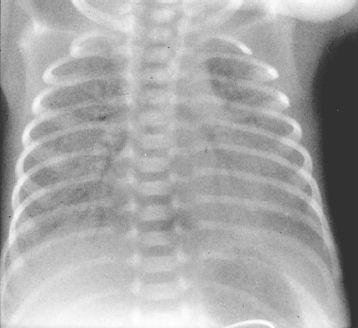
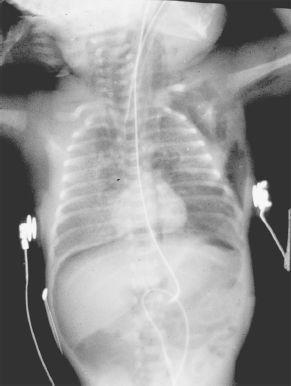
Two different strategies are used for administration of exogenous surfactant. Prophylactic surfactant may be given within 30 minutes after birth; rescue surfactant is given once the diagnosis of RDS is made by radiologic and clinical criteria. Umbilical lines are placed in premature babies for monitoring blood gases and for IV access. The chest radiograph in RDS shows a reticulogranular pattern with air bronchograms (
Figure 112-3A
). Severe respiratory distress appears as a “whiteout” (
Figure 112-3B
). Because the chest radiograph appearance of group B streptococcal pneumonia and surfactant deficiency are similar, any premature baby with respiratory distress should have a workup for possible sepsis, and antibiotic therapy should be initiated.