Pediatric Examination and Board Review (196 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

2.
(C)
Examination of a child for retinal hemorrhages requires the expertise of an ophthalmologist who can dilate the child’s eyes and perform a thorough examination of the retina. Ophthalmologic examination in this case reveals bilateral retinal hemorrhages (see
Figure 109-2
). The ophthalmologist will be able to document the number of hemorrhages, the layers they are contained in, and their extent. The ophthalmologist will also look for retinoschisis (a tear of the retina). Retinal hemorrhages are not necessary to diagnose traumatic brain injury, and they can be bilateral or unilateral. Classic findings for inflicted brain injury are retinal hemorrhages that involve multiple layers and extend out to the periphery. Retinal hemorrhages can last for weeks after an injury. After a period of healing, a child can appear well on clinical examination. An evaluation for retinal hemorrhages would be warranted if head trauma was suspected. Current data support the notion that cardiopulmonary resuscitation (CPR) does not cause retinal hemorrhage.
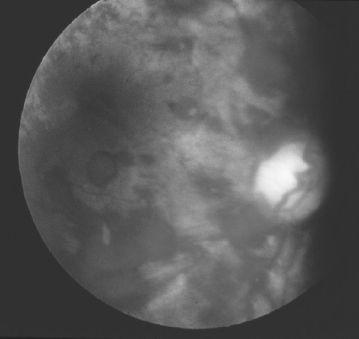
FIGURE 109-2.
Extensive retinal hemorrhages. See color plates.
3.
(C)
A head CT scan is more likely than an MRI to demonstrate an acute subarachnoid bleed. The preferred neuroimaging in a child with suspected head trauma should be a CT scan because of the ease with which it can be obtained. It will also be valuable because serial CT scans are often used to assess progression of a central finding. An MRI is indicated after the initial head CT in children with central injury because it is able to detect intracranial hemorrhages in various stages and also to better delineate the location of extra-axial hemorrhages (eg, subdural versus subarachnoid bleeding). The significance of a subdural hemorrhage must be analyzed within the context of the child’s examination, clinical status, and the history of the injury. It is important not to label a subdural bleed as pathognomonic for inflicted trauma. Epidural hemorrhages are pathognomonic because of impact injuries. A skull radiograph is the best study to visualize a skull fracture; skull fractures may also be seen on CT depending on the direction of the fracture in relation to the CT slices. If the fracture is parallel to the cuts of the CT, it may be missed. Most household falls do not cause more than a skin contusion or subgaleal bleed. A skull fracture in the temporoparietal area can result from an impact injury; it is also possible, but rare, to see an impact-induced subdural hemorrhage.
4.
(B)
A babygram is not sufficient to evaluate a child for occult skeletal injury; clinically relevant injuries such as metaphyseal injuries will be missed. A complete skeletal survey includes 19 views: anteroposterior (AP) views of the skull, thorax, pelvis, humeri, forearms, femurs, tibias, and feet, lateral views of the skull, cervical spine, thorax, lumbar spine, and oblique views of the hands. A bone scan augments a skeletal survey in that it can visualize injuries that are too acute to be seen on a skeletal survey and can aid in elucidating the difference between a normal variant and a traumatic injury. However, a bone scan is limited in its ability to age injuries and it requires injection of a radionuclide. The child must be still or sedated, and the scan must be directed by a radiologist to ensure the correct images are obtained. Improper views or images result in an inability to visualize injuries related to abuse in children.
5.
(D)
Male caretakers are at greater risk to inflict traumatic brain injury in an infant.
6.
(B)
All the choices except B are thought to increase the susceptibility of the infant brain to inflicted brain trauma.
7.
(A)
Depending on many factors, rib fractures will be visualized by radiograph in 7-10 days after the injury when there is healing and new bone formation. As this process continues with callus formation, rib fractures become visible. A technetium bone scan can visualize acute rib fractures within a few days of the injury, but there are limitations of this study as well (ie, it is more labor intensive, involves an injection, and cannot assist in aging the injury). Rib fractures are not known to result from cesarean delivery. In the case, because the rib fractures are callused and the mental status changes appear to be more acute, the head and rib trauma appear to have been inflicted at different times. It is important to acknowledge that our ability to age bleeding in the extra-axial space is limited.
8.
(D)
Classic metaphyseal fractures of the long bones (eg, bucket handle fractures or chip fractures) are injuries that are highly specific for child abuse. The mechanism for these injuries in infants is the application of rotational forces generated as an infant is shaken by the trunk or when the child’s extremity is used as a handle for shaking the child. Classic metaphyseal injuries most often do not present with pain and do not require treatment. They occur near the joints of the long bones.
9.
(E)
The age of the patient and the belief that a sibling was allegedly responsible for the injury make “E” the best choice. Any fracture in nonambulatory children should instigate an investigation because, developmentally speaking, accidental fractures are very rare in this age group regardless of the morphology of the fracture. Once children are ambulatory they are then able to generate forces required to sustain skeletal injuries. Thus, the morphology of the fracture is less of a concern than the age of the child, and, in fact, transverse fractures are more common than spiral fractures in the nonambulatory child.
10.
(D)
Delay in seeking care, discrepancies in the history of the injury, injuries caused by a sibling, and inconsistencies between the child’s developmental abilities and the sustained injury focus investigational efforts toward evaluating the consistency of the injury and the history. If a parent is disheveled or smells of alcohol, this has implications with regard to child welfare issues, but it does not diagnose an inflicted injury.
11.
(C)
Protection of a hospitalized child from further injury while an investigation for maltreatment is in progress is a priority for the hospital and medical staff. Restriction of visitation should be discussed with the child welfare investigator.
12.
(E)
Because this child has healing rib fractures, one would want to review the medical presentation and evaluation of the prior episode of gastroenteritis. The diagnosis of inflicted head trauma can be missed by the treating physician because of the lack of external findings of trauma; the symptoms of CNS injury can often masquerade as a viral syndrome or gastroenteritis. A study by Jenny et al indicates that 30% of children with abusive head trauma had a prior head injury that was not diagnosed.
13.
(B)
Many studies show that minor falls from less than 3 feet do not cause significant intracranial injury. The lack of a cutaneous finding of an impact does not rule out an impact injury. Tin ear syndrome involves rotational injuries and includes unilateral internal ear injury and intracranial bleeding. The force necessary to cause inflicted traumatic brain injury (eg, previously called the “shaken baby syndrome”) is out of the realm of normal caretaking behavior and resuscitation efforts.
14.
(D)
Diaphyseal fractures are not typical of the shearing injuries associated with violent shaking of an infant, although classic metaphyseal fractures are.
15.
(B)
Abusive head trauma is the leading cause of death from trauma in infancy. All children with brain trauma need to have high-risk developmental follow-up because of irreversible brain injury, which may be manifested as cognitive delays or behavioral problems.
16.
(B)
The GCS is a universally used assessment tool to aid in assessing the severity of a central injury. The scale has 3 examination categories: eye, motor, and verbal response. Scores range from 3 to 15. Rules for use of the GCS system differ based on age of the patient.
17.
(D)
A head CT scan should be the first line of imaging, not an MRI.
18.
(C)
Cognitive impairment is difficult to assess in this child because the diagnosis of traumatic brain injury was occult. This differs from the situation with witnessed or “accidental” brain injury where the mechanism of injury is clear. In this circumstance the amount of time before medical intervention is sought decreases the likelihood and extent of secondary brain injury (eg, development of cerebral edema and injury from untreated hypoxia).
 S
S
UGGESTED
R
EADING
Jenny C, Hymel KP, Ritzen A, et al. Analysis of missed cases of abusive head trauma.
JAMA.
1999;282(7):621-626.
Kellogg ND; American Academy of Pediatrics Committee on Child Abuse and Neglect. Evaluation of suspected child physical abuse.
Pediatrics.
2005;119:1232-1241.
Reece RM, Christian CW, eds.
Child Abuse
:
Medical Diagnosis and Management
. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009.
CASE 110: A 6-YEAR-OLD WITH VAGINAL DISCHARGE
A 6-year-old girl is brought to your office for evaluation of malodorous blood-tinged vaginal discharge. The mother noted scant discharge on her daughter’s underwear for 1 week. The child has not had any fever, although she did have a stomachache 1 week ago. There was no history of vomiting, diarrhea, constipation, or dysuria. The child has taken more frequent baths for the last 3 weeks because she is now participating in sports. She lives with her mother and sister; her parents are divorced but she does have weekend visits with her father. She has been a good student, although her school performance declined after the divorce. The mother feels her daughter is currently doing well at school.
