Ross & Wilson Anatomy and Physiology in Health and Illness (80 page)
Read Ross & Wilson Anatomy and Physiology in Health and Illness Online
Authors: Anne Waugh,Allison Grant
Tags: #Medical, #Nursing, #General, #Anatomy

Acute subdural haemorrhage
This is due to haemorrhage from small veins in the dura mater or from larger veins between the layers of dura mater before they enter the venous sinuses. The blood may spread in the subdural space over one or both hemispheres (
Fig. 7.49A
). There may be concurrent subarachnoid haemorrhage (
Fig. 7.49B
), especially when there are extensive brain contusions and lacerations.
Chronic subdural haemorrhage
This may occur weeks or months after minor injuries and sometimes there is no history of injury. It occurs most commonly in people in whom there is some cerebral atrophy, e.g. older people and in alcoholism. Evidence of increased ICP may be delayed when brain volume is reduced. The haematoma formed gradually increases in size owing to repeated small haemorrhages and causes mild chronic inflammation and accumulation of inflammatory exudate. In time it is isolated by a wall of fibrous tissue.
Intracerebral haemorrhage and cerebral oedema
These occur following contusions, lacerations and shearing injuries associated with acceleration and deceleration, especially rotational movements.
Cerebral oedema
(
p. 173
) is a common complication of contusions of the brain, leading to increased ICP, hypoxia and further brain damage.
Meningitis
Inflammation of the meninges may occur following a compound fracture of the skull that is accompanied by leakage of CSF and blood from the site, providing a route of entry for microbes. The escape of CSF and blood may be through the:
•
skin, in compound skull fractures
•
middle ear, in fractures of the temporal bone (
CSF otorrhoea
)
•
nose, in fractures of sphenoid, ethmoid or frontal bones when the air sinuses are involved (
CSF rhinorrhoea
).
Post-traumatic epilepsy
This is usually characterised by seizures (fits) and may develop in the first week or several months after injury. Early development is most common after severe injuries, although in children the injury itself may have appeared trivial. After depressed fractures or large haematomas epilepsy tends to develop later.
Persistent vegetative state
In this condition there is severe brain damage that results in unconsciousness but the vital centres that control homeostasis remain intact, e.g. breathing, blood pressure.
Cerebral hypoxia
Hypoxia may be due to:
•
disturbances in the autoregulation of blood supply to the brain
•
conditions affecting cerebral blood vessels.
When the mean blood pressure falls below about 60 mmHg, the autoregulating mechanisms that control the blood flow to the brain by adjusting the diameter of the arterioles fail. The consequent rapid decrease in the cerebral blood supply leads to hypoxia and lack of glucose. If severe hypoxia is sustained for more than a few minutes there is irreversible brain damage. The neurones are affected first, then the neuroglial cells and later the meninges and blood vessels. Conditions in which autoregulation breaks down include:
•
cardiorespiratory arrest
•
sudden severe hypotension
•
carbon monoxide poisoning
•
hypercapnia (excess blood carbon dioxide)
•
drug overdosage with, e.g., opioid analgesics, hypnotics.
Conditions affecting cerebral blood vessels that may lead to hypoxia include:
•
occlusion of a cerebral artery by, e.g., a rapidly expanding intracranial lesion, atheroma, thrombosis or embolism (
Ch. 5
)
•
arterial stenosis that occurs in arteritis, e.g. polyarteritis nodosa, syphilis, diabetes mellitus, degenerative changes in older people.
If the individual survives the initial episode of ischaemia, then infarction, necrosis and loss of function of the affected area of brain may occur.
Stroke (cerebrovascular disease)
This condition is a common cause of death and disability, especially in older people. Predisposing factors include:
•
hypertension
•
atheroma
•
cigarette smoking
•
diabetes mellitus.
It occurs when blood flow to the brain is suddenly interrupted, causing hypoxia. The effects include paralysis of a limb or one side of the body and disturbances of speech and vision. The nature and extent of damage depend on the size and location of the affected blood vessels. The main causes are cerebral infarction (approx. 85%) and spontaneous intracranial haemorrhage (15%).
Cerebral infarction
This is caused by atheroma complicated by thrombosis (
p. 112
) or blockage of an artery by an embolus from, e.g., infective endocarditis. The cerebral hemispheres are usually affected. When complete recovery occurs within 24 hours, the event is called a
transient ischaemic attack
(TIA). Recurrence or
completed stroke
associated with permanent damage may follow.
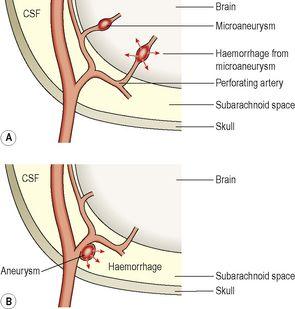
Spontaneous intracranial haemorrhage
The haemorrhage may be into the subarachnoid space or intracerebral (
Fig. 7.50
). It is commonly associated with an aneurysm or hypertension. In each case the escaped blood may cause arterial spasm, leading to ischaemia, infarction, fibrosis (gliosis) and hypoxic brain damage. A severe haemorrhage may be instantly fatal while repeated small haemorrhages have a cumulative effect in extending brain damage (
multi-infarct dementia
).
Figure 7.50
Types of haemorrhage causing stroke: A.
Intracerebral.
B.
Subarachnoid.
Intracerebral haemorrhage
Prolonged hypertension leads to the formation of multiple microaneurysms in the walls of very small arteries in the brain. Rupture of one or more of these, due to continuing rise in blood pressure, is usually the cause of intracerebral haemorrhage. The most common sites are branches of the middle cerebral artery in the region of the internal capsule and the basal ganglia.
Severe haemorrhage
This causes compression and destruction of tissue, a sudden increase in ICP and distortion and herniation of the brain. Death follows when the vital centres in the medulla oblongata are damaged by haemorrhage or if there is coning due to increased ICP.
Less severe haemorrhage
This causes paralysis and loss of sensation of varying severity, affecting the side of the body opposite the haemorrhage. If the bleeding stops and does not recur a fluid-filled cyst develops, i.e. the haematoma is walled off by gliosis, the blood clot is gradually absorbed and the cavity filled with tissue exudate. When the ICP returns to normal some function may be restored, e.g. speech and movement of limbs.
Subarachnoid haemorrhage
This is usually due to rupture of a berry aneurysm on one of the major cerebral arteries, or bleeding from a congenitally malformed blood vessel (
Fig. 7.50B
). The blood may remain localised but usually spreads in the subarachnoid space round the brain and spinal cord, causing a general increase in ICP without distortion of the brain (
Fig. 7.49B
). The irritant effect of the blood may cause arterial spasm, leading to ischaemia, infarction, gliosis and the effects of localised brain damage. It occurs most commonly in middle life, but occasionally in young people owing to rupture of a malformed blood vessel. This condition is often fatal or results in permanent disability.
Dementia
Dementia is caused by progressive, irreversible degeneration of the cerebral cortex and results in mental deterioration, usually over several years. There is gradual impairment of memory (especially short term), intellect and reasoning but consciousness is not affected. Emotional lability and personality change may also occur.
Alzheimer’s disease
This condition is the commonest form of dementia in developed countries. The aetiology is unknown although genetic factors may be involved. Females are affected twice as often as males and it usually affects those over 60 years, the incidence increasing with age. There is progressive atrophy of the cerebral cortex accompanied by deteriorating mental functioning. Death usually occurs between 2 and 8 years after onset.
Huntington’s disease
This usually manifests itself between the ages of 30 and 50 years. It is inherited as an autosomal dominant disorder (see
p. 433
) associated with deficient production of the neurotransmitter gamma aminobutyric acid (GABA). By the time of onset, the individual may have passed the genetic abnormality on to their children. Extrapyramidal changes cause chorea, rapid uncoordinated jerking movements of the limbs and involuntary twitching of the facial muscles. As the disease progresses, cortical atrophy causes personality changes and dementia.
Secondary dementias
Dementia may occur in association with other diseases:
•
cerebrovascular disease, e.g. multi-infarct dementia
•
infections, e.g. neurosyphilis, human immunodeficiency virus (HIV), Creutzfeldt–Jakob disease
•
cerebral trauma
•
alcoholism and some drugs
•
vitamin B deficiencies
•
metabolic disorders, e.g. hypothyroidism, uraemia, liver failure.
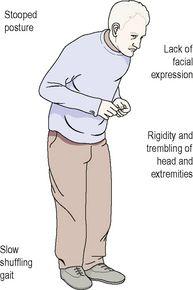
Parkinson’s disease
In this disease there is gradual degeneration of dopamine releasing neurones in the extrapyramidal system. This leads to lack of control and coordination of muscle movement resulting in:
•
slowness of movement (bradykinesia) and difficulty initiating movements
•
fixed muscle tone causing expressionless facial features, rigidity of voluntary muscles causing the slow and characteristic stiff shuffling gait and stooping posture
•
muscle tremor of extremities that usually begins in one hand, e.g. ‘pill rolling’ movement of the fingers.
Onset is usually between 45 and 60 years. The cause is usually unknown but some cases are associated with repeated trauma as in, e.g., ‘punch drunk’ boxers; tumours causing midbrain compression; drugs, e.g. phenothiazines; heavy metal poisoning. There is progressive physical disability but the intellect is not impaired (
Fig. 7.51
).