Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (73 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

•
Nonclassical
(5%): nodular lymphocyte predominant (NLP); involves peripheral LN
80% present in stages I–II and Rx can be RT alone or combination chemo + RT w/ 80% 10-y progression-free survival, 93% overall survival (
JCO
1997;15:3060)
Consider rituximab as most NLP RS cells are CD20+
Stages III–IV treated with combination chemo (see below)
Treatment
(
Lancet
2012;380:836)
•
Stages I–II
:
ABVD
(doxorubicin, bleomycin, vinblastine, dacarbazine) ± RT
Lower intensity regimens comparable efficacy if favorable prognosis (
NEJM
2010;363:640)
•
Stages III–IV
:
ABVD
× 6 cycles or
escalated BEACOPP
(bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine and prednisone) • Refractory/relapsed disease: salvage chemo + auto HSCT, ± RT
• Late effects include ↑ risk for:
second cancers
:
breast
(if RT), ∴ annual screening at age 40 or 8–10 y post RT;
lung
, ? role of screening CXR or CT (controversial);
acute leukemia/MDS
;
NHL
cardiac disease
(if RT or anthracycline), ? role of echo/stress at 10 y (controversial)
pulmonary toxicity
(if bleomycin)
hypothyroidism
(if RT), ∴ annual TSH (if neck RT)
NON-HODGKIN LYMPHOMA (NHL)
Epidemiology and risk factors
•
70,000 new cases/y; median age at dx
65 y;predominance; 85% B-cell origin • Associated conditions: immunodeficiency (eg, HIV, posttransplant); autoimmune disorders (eg, Sjögren’s, RA, SLE); infection (eg, EBV, HTLV-I,
H. pylori
) • Burkitt’s lymphoma: (1) endemic or African (jaw mass, 80–90% EBV-related); (2) sporadic or American (20% EBV-related); (3) HIV-related
Treatment
(
Lancet
2012;380:848)
• Treatment and prognosis determined by histopathologic classification rather than stage • Rituximab (antibody to CD20;
NEJM
2012;366:2008) if CD20+; no role if tumor is CD20– •
Indolent:
goal is sx management (bulky dis., cytopenias, “B” sx); not curable w/o allo HSCT
Options include radiation for localized disease, rituximab ± chemo (bendamustine, CVP, fludarabine)
For MALT → treat
H pylori
if
Rituximab maintenance ↑ survival in relapsed disease (
JNCI
2009:101:248); growing role for rituximab maintenance in indolent and aggressive disease (
Lancet
2011;377:42)
•
Aggressive
(DLBCL, 30–40% of NHL): goal is cure (
JCO
2005;23:6387)
R-CHOP
(
r
ituximab,
c
yclophosphamide, doxorubicin =
h
ydroxydaunorubicin, vincristine =
O
ncovin,
p
rednisone) (
NEJM
2002;346:235 & 2008;359:613) 10-y progression-free survival = 45%; overall survival = 55% (
Blood
2010;116:2040)
? R-ACVBP (
r
itux, doxorubicin =
A
driamycin,
c
yclophosph,
v
indesine,
b
leo,
p
rednisone) ↑ 3-y OS vs. R-CHOP, but ↑ adverse events (
Lancet
2011;378:1858)
+
Radiation
for localized or bulky disease
Consider
CNS prophylaxis
w/ intrathecal or systemic high-dose methotrexate if paranasal sinus, testicular, breast, periorbital, paravertebral or bone marrow involved; ≥2 extranodal site + ↑ LDH may also warrant
Refractory/relapsed disease: salvage chemo; high-dose chemo + auto-HSCT (
NEJM
1995;333:1540); allo-HSCT if beyond 2nd relapse
•
Highly aggressive
Burkitt’s: intensive short-course chemotherapy (
Blood
2004;104:3009)
Low risk defined as nl LDH & single focus of disease <10 cm; all others high risk
Low risk Rx = CODOX-M (cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate ± rituximab) (
Leuk Lymph
2004;45:761)
High risk Rx = CODOX-M/IVAC (above w/ ifosfamide, etoposide, high-dose cytarabine), hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)
All Pts receive CNS prophylaxis & tumor lysis syndrome prophylaxis
Lymphoblastic lymphoma (B or T cell): treated like ALL (see “Acute Leukemia”)
Prognosis
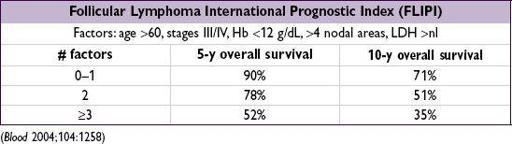
• Indolent: typically incurable, but long median survival
• Aggressive: ↑ chance of cure, but overall worse prognosis
HIV-associated NHL
(
Blood
2006;107:13)
• HIV imparts 60–100× relative risk • NHL is an AIDS-defining malignancy along with Kaposi’s, cervical CA, anal CA • Concurrent HAART & chemotherapy likely provide survival benefit • DLBCL & immunoblastic lymphoma (67%): CD4 <100, EBV-associated Treat as immunocompetent (CHOP-R), but avoid rituximab if CD4 <100 Alternative regimens include R-EPOCH (etop, pred, vincristine, cyclophos, doxorubicin) • Burkitt’s (20%): can occur with CD4 >200 Treat as immunocompetent; prognosis is not significantly worse • Primary CNS lymphoma (16%): CD4 <50, EBV-associated (also seen in Pts w/o HIV) Treat with high-dose methotrexate + steroids ± RT
imparts 60–100× relative risk • NHL is an AIDS-defining malignancy along with Kaposi’s, cervical CA, anal CA • Concurrent HAART & chemotherapy likely provide survival benefit • DLBCL & immunoblastic lymphoma (67%): CD4 <100, EBV-associated Treat as immunocompetent (CHOP-R), but avoid rituximab if CD4 <100 Alternative regimens include R-EPOCH (etop, pred, vincristine, cyclophos, doxorubicin) • Burkitt’s (20%): can occur with CD4 >200 Treat as immunocompetent; prognosis is not significantly worse • Primary CNS lymphoma (16%): CD4 <50, EBV-associated (also seen in Pts w/o HIV) Treat with high-dose methotrexate + steroids ± RT