Pediatric Examination and Board Review (84 page)
Read Pediatric Examination and Board Review Online
Authors: Robert Daum,Jason Canel

(D) A and B
(E) B and C
5.
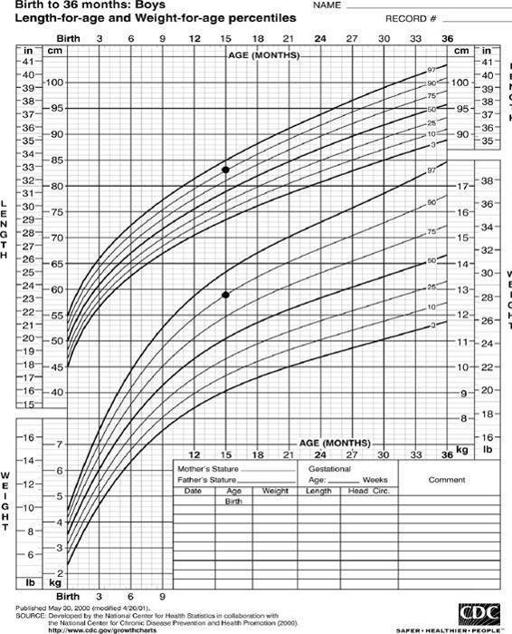
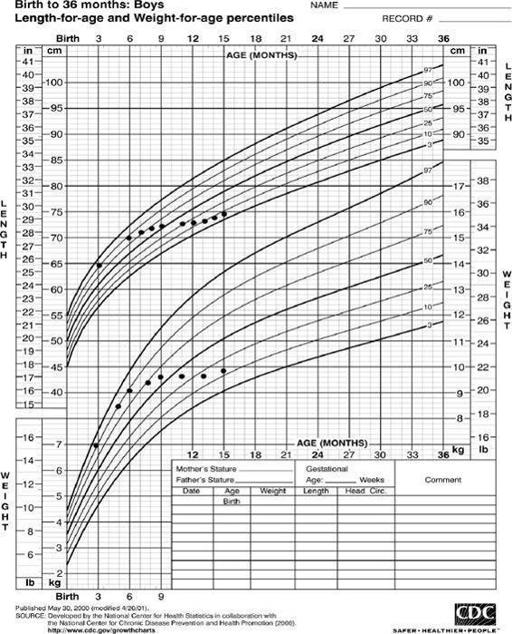
If the growth curve for the child in the vignette was the curve in
Figure 52-2
, your concern would be
(A) celiac disease
(B) early Crohn disease
(C) chronic
Giardia
infection
(D) growth hormone deficiency
(E) CF
6.
The laboratory studies that would allow you to make the diagnosis include
(A) hydrogen breath test
(B) CBC, sedimentation rate, and serum albumin
(C) tissue transglutaminase IgA
(D) pANCA
(E) A and C
7.
Treatment for celiac disease includes
(A) gluten-free diet
(B) evaluation for hypothyroidism
(C) evaluation for anemia
(D) all of the above
(E) none of the above
8.
In a child with a history of growth failure associated with rectal prolapse and chronic diarrhea, which of the following tests would likely be abnormal?
(A) stool examination for ova and parasites
(B) stool evaluation for reducing substances
(C) stool evaluation for fat content
(D) stool culture
(E) all of the above
9.
The most appropriate next test for the child in question 8 is
(A) abdominal radiograph
(B) barium enema
(C) sweat test
(D) endoscopy
(E) food allergy testing
10.
Later in life, the child in question 8 may suffer from
(A) constipation
(B) distal intestinal obstruction syndrome (DIOS; a meconium ileus equivalent)
(C) focal biliary cirrhosis
(D) GERD
(E) all of the above
11.
If the patient was 5 years old and had a history of duodenal atresia repair, the additional tests you would order include
(A) upper GI series with small bowel follow-through
(B) hydrogen breath test
(C) endoscopy with biopsy
(D) upper endoscopy with biopsy
(E) CT scan of the abdomen and pelvis with triple contrast
12.
If the child had stools that “burned,” the likely malabsorption would be
(A) carbohydrate
(B) fats
(C) proteins
(D) vitamins and minerals
(E) bicarbonate
13.
If the stools were described as covered with mucus and were heme positive, the patient’s history would likely include
(A) exposure to well water
(B) exposure to antibiotics
(C) exposure to other ill children
(D) family history of inflammatory bowel disease
(E) history of lactose intolerance
14.
The antibiotic that most often leads to
C difficile
infection in pediatric patients is
(A) amoxicillin
(B) clindamycin
(C) erythromycin
(D) cefdinir
(E) all of the above cause an equal incidence of
C difficile
15.
If the child was 6 week old with 5 loose watery stools with blood daily, the most likely diagnosis is
(A) infectious colitis
(B) protein intolerance
(C) lactose intolerance
(D) congenital C1-losing diarrhea
(E) fat malabsorption
16.
If the child was feeding on a cow’s milk lactosecontaining formula, the treatment would be
(A) soy formula
(B) hydrolyzed formula
(C) cow’s milk lactose-free formula
(D) await stool culture results before making recommendations
(E) await stool electrolytes before making recommendations
17.
If the child in question 15 was being breast-fed, then the treatment would be
(A) soy formula
(B) hydrolyzed formula
(C) await stool cultures
(D) restrict the cow’s milk in Mom’s diet
(E) lactose-free formula
18.
A microbiology lab calls you with a report of a positive
C difficile
toxin result on a 10-day-old patient of yours. Your treatment plan would be
(A) extended and more aggressive compared with older children because of the increased chance of catastrophic complications in this age group
(B) the same as older children because age has no effect on the chance of catastrophic complications
(C) shortened compared with older children because of the decreased chance of catastrophic complications in this age group
(D) to retest to confirm diagnosis before beginning therapy
(E) no treatment is indicated
ANSWERS
1.
(E)
The initial evaluation of a child with chronic diarrhea should concentrate on the history and physical examination. This child is healthy and growing normally in all respects. This is typical of toddler’s diarrhea and should be handled with education and reassurance. The screening laboratory tests listed are examinations of the stool looking for malabsorption and intestinal infection; these diagnoses would not be suspected in this patient from the history or physical examination.
2.
(A)
A 15-month-old child who has normal growth and diarrhea without accompanying GI symptoms likely has nonspecific diarrhea of childhood. Parents will frequently see food in the stool. The symptoms of carbohydrate malabsorption are detailed below. There was no history of gastroenteritis before the onset of this diarrhea.
3.
(D)
Nonspecific diarrhea of childhood can occur because of any of the dietary problems listed. Children can have increased diarrhea if they are put on a clear liquid diet frequently.
4.
(A)
Reassurance and restricting the dietary excesses are the best initial treatments.
5.
(A)
This is a classic growth curve for celiac disease. This patient’s growth retardation began at approximately 6 months of age, which is typically when gluten-containing foods are introduced to the diet. It would be very unusual for Crohn disease to present at 6 months of age. CF would very likely cause malnutrition from birth.
6.
(C)
The evaluation of a child suspected to have celiac disease initially should be serologic. Detection of antigliadin antibodies is a sensitive test but not specific to Celiac disease, and these antibodies can be present in other GI diseases. Detection of antiendomysial antibodies is much more specific. Tissue transglutaminase is a specific antiendomysial antibody. Caution should be used in interpretation because 2-5% of celiac patients are IgA deficient and have a false-negative test result.
7.
(D)
The treatment for celiac disease is a gluten-free diet. These patients also have a high incidence of associated hypothyroidism and iron deficiency anemia.
8.
(C)
A patient with diarrhea, growth failure, and rectal prolapse has CF until proven otherwise. The fat content in the stool will be abnormal secondary to pancreatic insufficiency that commonly occurs in CF patients.
9.
(C)
A sweat test should be done to ensure the clinical findings are from CF. Although gene testing for CF is readily available and may aid in predicting long-term prognosis and genetic counseling, a properly performed sweat test can provide a rapid and accurate diagnosis that allows for immediate initiation of therapies. Without other signs or symptoms, imaging studies, endoscopy, and allergy testing are not indicated.
10.
(E)
Later in life, children with CF can suffer from multiple GI symptoms. Constipation and GERD are commonly associated symptoms. DIOS presents with partial or complete bowel obstruction. It responds to medical therapy with gastrografin enemas. It can recur. In chronic cases, it is important to ensure there is adequate pancreatic enzyme replacement. About 2-3% of CF patients develop biliary cirrhosis.
11.
(B)
Patients with previous bowel surgery are predisposed to have bacterial overgrowth. This can be diagnosed with a breath hydrogen test. The patient ingests sugar that bacteria convert into hydrogen. In small bowel bacterial overgrowth, the peak of expired hydrogen will be early because the bacteria are in the small bowel, not the colon. In carbohydrate malabsorption there will be a later peak when the unabsorbed sugar reaches the colon. Without signs of obstruction or perforation, radiographic studies are not indicated. Endoscopy would not aid in this diagnosis.
12.
(A)
Carbohydrate malabsorption leads to delivery of unabsorbed carbohydrate to the colon. The bacteria in the colon convert it to acid. Reducing substances will be positive.
