Resident Readiness General Surgery (74 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

POSTOPERATIVE WOUND COMPLICATIONS
Answers
1.
Wound classification is based on the degree of wound contamination. Consider the difference in exposure to bacterial load between an incision made for an inguinal hernia repair and an exploratory laparotomy for a penetrating abdominal trauma with numerous small bowel and colon injuries. In the former, proper
sterile technique should essentially eliminate bacterial contamination from the surgical site. In the latter, however, bacterial contamination of the incision site secondary to gross spillage of stool into the abdomen is virtually inevitable, making the risk of postoperative wound infection considerably higher.
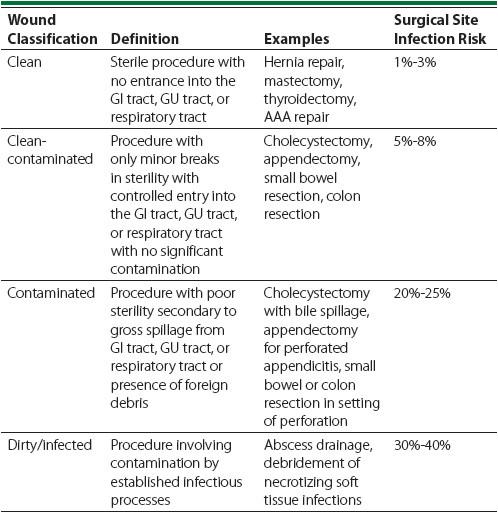
Wound classification is an important concept for any surgeon to understand, as it often drives clinical decision making. For example, wound classification is fundamental in deciding how or even if to close a wound at the end of a case. Additionally, classifying wounds based on their degree of contamination provides a mechanism for postoperative wound infection risk stratification. Such a tool makes it possible to maintain appropriate levels of suspicion for wound infection when evaluating a postoperative patient with a fever, leukocytosis, or peri-incisional erythema. For a description of the wound classification system most commonly used, see
Table 57-1
.
Table 57-1.
Wound Classification and Surgical Site Infection Risk
2
. While the degree of contamination is one of the determining factors, it should be noted that there are multiple other factors that can influence the rate of SSIs. These include the use of preoperative antibiotics, maintaining normothermia, maintaining euglycemia, patient factors such as immunocompromise, and modifications to surgical technique that can be made to reduce contamination. As an intern, the first two items deserve special attention as they are sometimes solely your responsibility. Hyperglycemia is also often under your purview, but complicated enough that it gets its own chapter.
Preoperative Antibiotics
Even in a clean case a skin incision obligatorily exposes vulnerable subcutaneous tissues to a bacterial challenge. Bugs love it if you inevitably sprinkle these subdermal spaces with pockets of the patient’s blood—essentially blood agar incubated at 37°C. Your goal, therefore, is to synchronize the antibiotic “peak” with the skin incision. Preoperative antibiotics should be infused during the 1-hour window prior to the skin incision and every 3 to 4 hours (2-3 antibiotic half-lives) during longer procedures.
Normothermia
Trauma surgeons are exquisitely sensitive to the link between hypothermia and bleeding (the coagulation cascade is impaired by hypothermia). However, there are also antiseptic advantages to normothermia (or even hyperthermia—this is why we get a fever with infection). If you wheel your patient into the recovery room/PACU following a bowel resection, with a temperature of only 2° below normal (34.5°C), the chances of a wound infection double. Maintain your patient’s core temperature above 36.5°C.
3.
A seroma is a collection of liquefied fat, serum, and lymphatic fluid located underneath a surgical incision. These typically present with pressure, discomfort, and sometimes drainage of clear fluid from a well-circumscribed area of swelling around a surgical incision. Seromas most frequently develop following procedures that require elevation of skin flaps and transection of lymphatic channels.
A hematoma is an abnormal collection of blood and/or clot in a wound and is one of the most common wound complications seen in surgical patients. Most hematomas are caused by incomplete intraoperative hemostasis. Hematomas manifest differently based on their size, location, and underlying etiology. Generally, hematomas present as swelling and/or pain in the area of an incision. Discoloration of the wound edges and sometimes blood leaking through the incision may also be seen. It is essential to look for signs of hematoma expansion, particularly in the neck, where rapid expansion can lead to airway compromise.
Although both seromas and hematomas are risk factors for the development of postoperative wound infection (and they may in fact be associated with very similar signs), they are not themselves infections. SSIs are the result of contamination of the surgical site with microorganisms and are marked by a clinical presentation with features different from seromas and hematomas. Special attention must be paid to the presence of crepitus or pain out of proportion with other physical exam findings, as these are ominous signs of necrotizing soft tissue infection. If this diagnosis is missed, it can become fatal within hours. See Chapter 45 on this topic for more information.
This patient most likely does have a wound infection given his elevated temperature as well as the constellation of other signs and symptoms. While pain, drainage, and erythema are individually nonspecific, in combination they are suggestive of infection. His leukocytosis must be evaluated in the context of his previous lab values, and if it is higher than his discharge white count, it too would suggest infection.
4.
Fundamental to the understanding of SSIs—and knowing the indications for imaging—is recognizing the depth of infection. SSIs are categorized into three groups: superficial incisional SSIs, deep incisional SSIs, and organ/space SSIs. Superficial incisional SSIs involve the skin, while deep incisional SSIs involve the fascia and muscle layers. Organ/space SSIs involve the organs or spaces that were opened up during the procedure. These include infections such as intra-abdominal abscess, hepatic abscess, and mediastinitis. This classification scheme is depicted in
Figure 57-1
.
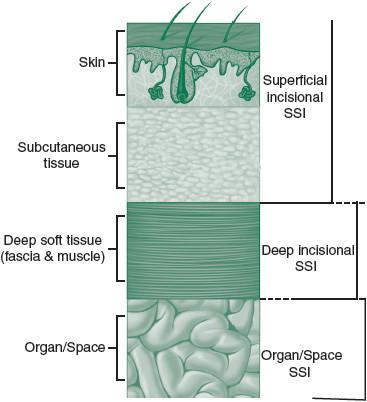
Figure 57-1.
Cross-section of abdominal wall depicting the anatomy and classification of surgical site infections. (Reproduced, with permission, from Hoffman BL, Schorge JO, Schaffer JI, et al.
Williams Gynecology
. 2nd ed. New York: McGraw-Hill; 2012. Figure 3-21.)
Superficial incisional SSIs typically develop 3 to 6 days after surgery, but this may vary. Symptoms often include erythema, tenderness, edema, and purulent drainage from the wound. Unlike seromas and hematomas, a patient with a wound infection may also have a low-grade fever and/or a leukocytosis, similar to the patient in this case. On exam, the wound may be soft or fluctuant. Surgical site pain that worsens or fails to resolve within 7 to 10 days of surgery is a subtle, but important marker for occult infection.
Deep incisional and organ/space SSIs tend to become apparent later in the postoperative course. These may remain occult or present with symptoms that mimic superficial SSIs, which can delay diagnosis and lead to significant complications. Deep incisional SSIs typically present with pain that extends beyond what would be expected from a surgical wound and beyond any margin of superficial erythema. Symptoms of organ/space SSIs are typically related to involved organ systems. Examples include diarrhea, prolonged or recurrent return of ileus after an operation, or pain on rectal exam.
The diagnosis of superficial postoperative wound complications is primarily made by physical exam as described above. The diagnosis of deep wound complications is more difficult, as their signs and symptoms are often less clear. In cases where there is suspicion for wound complication but no definitive
diagnosis, imaging studies can be obtained. However, as with any studies, they should only be obtained if the result could alter clinical decision making.
Ultrasonography is a noninvasive, inexpensive, and often readily available tool for assessing subcutaneous wound complications. Ultrasound may be useful in identifying subcutaneous fluid collections in need of drainage in patients where physical exam is difficult (ie, in the obese). CT scans are rarely indicated in the evaluation of superficial or deep incisional SSIs, with the notable exception of when there is suspicion that the SSI is actually a manifestation of an underlying organ/space infection.
Although clinical presentation and physical exam can point toward organ/space SSIs, the diagnosis is often unclear. CT scan is often the most useful modality for identifying organ/space infections. Like in incisional SSIs, obtaining an imaging study should only be done if the results of the study would drive management (ie, identifying an intra-abdominal abscess that would subsequently be drained). When considering obtaining a postoperative CT scan, it is important
to take into consideration the timing of the study. In the days following surgery, it is common for fluid to be present within the abdomen. Abscesses do not typically form until approximately postoperative days 5 to 7. Thus, a CT scan on postoperative day 3 is unlikely to provide useful information, as differentiating between normal postoperative fluid and an early abscess is often not possible. However, should concern for organ/space complications arise on postoperative day 5 or later, a CT scan is far more likely to provide useful information.
The type of CT scan is also important. Oral and intravenous contrasts make for an ideal radiographic evaluation of the abdomen for a source of postoperative organ/space SSIs. Oral contrast helps delineate the anatomy of the gastrointestinal tract. Additionally, extravasation of oral contrast into the abdomen is diagnostic of a leak. Intravenous contrast optimizes visualization of vascular structures and can identify a source of active bleeding. It can also help identify abscesses, which demonstrate peripheral rim enhancement when this type of contrast is administered.
A suspicion of leak may necessitate a dynamic study, such as a small bowel follow-through or a gastrographin enema. While CT scans are not the gold standard for determination of an anastomotic leak, they are frequently used due to their accessibility and comfort for patients.
For this patient, the exam and time course support the diagnosis of a superficial incisional SSI. Ultrasound is a viable imaging modality, although it is most useful when it is not already clear where to open the wound to drain the fluid. If this was later in the patient’s course and/or there were any other indications that this might be an organ/space SSI, then CT would instead be indicated.
5.
The most important principle in the management of suspected postoperative wound infections is to open the wound over the area of infection. Opening an infected wound makes several things possible. First, it allows for evacuation and persistent drainage of purulent, microorganism-laden fluid. This alone markedly decreases the bacterial load within an infected wound. Opening an infected wound also permits local wound exploration with a cotton-tipped applicator. Wound exploration makes it possible to identify and debride any nonviable tissue and assess the integrity of the underlying fascia. Debriding nonviable tissue is an important component of managing wound infections because dead tissue provides an ideal site for bacterial proliferation that is not readily penetrated by host defense mechanisms. Assessing fascial integrity is important because wound infection is a risk factor for fascial dehiscence. Additionally, fascial compromise may also be indicative of a more deeply rooted infectious process such as an intra-abdominal abscess that may require more significant intervention. Any persistent, heavy drainage of serous fluid should raise suspicion of fascial dehiscence, as this serous fluid may very well be peritoneal fluid. This essentially always warrants more extensive evaluation and having a senior resident involved is paramount.
Generally speaking, infected wounds that have been opened should remain open and be allowed to heal by secondary intention. This allows for frequent wet-to-dry dressing changes, continuous drainage from the wound, and prevention of purulent fluid reaccumulation. Along the same lines, the suprafascial portion of surgical wounds at a particularly high risk for infection may be preemptively left open in order to decrease the likelihood that a postoperative wound infection will develop. Although healing by secondary intention generates a significant wound care need for a prolonged period of time, it is often an essential component of postoperative wound infection management and is the standard approach.
